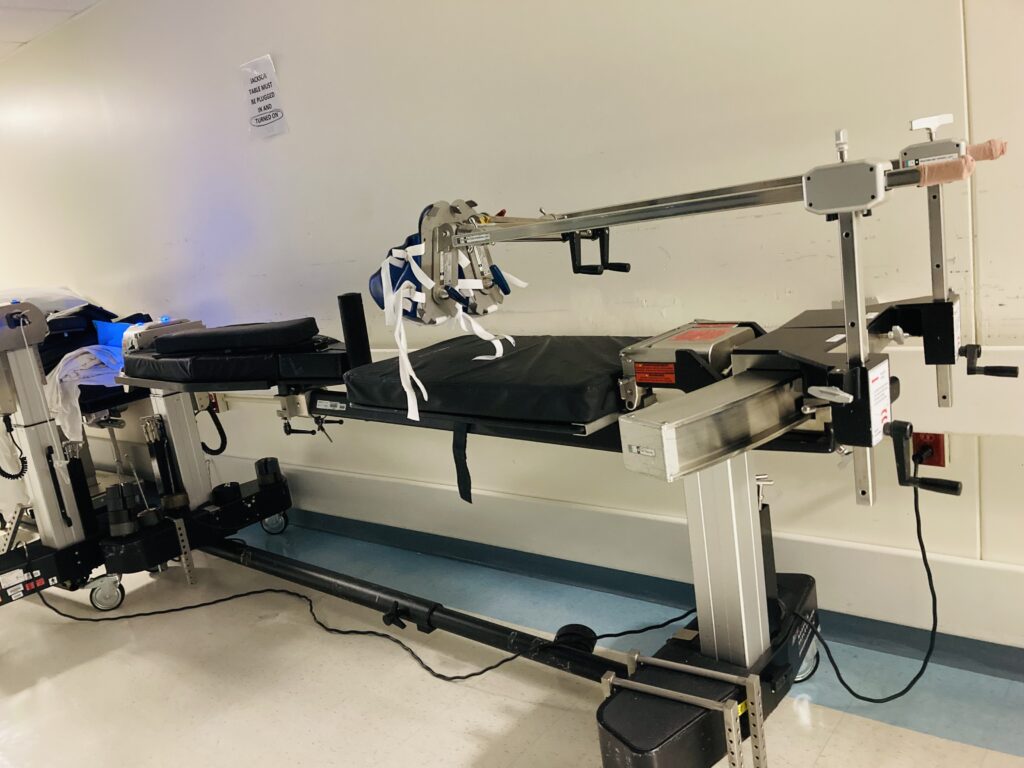
The Jackson table is a type of operating room bed that has many attachments to help with different surgeries in different positions. The Wilson frame is a medical device used to keep a patient lying face down (prone) during surgery.
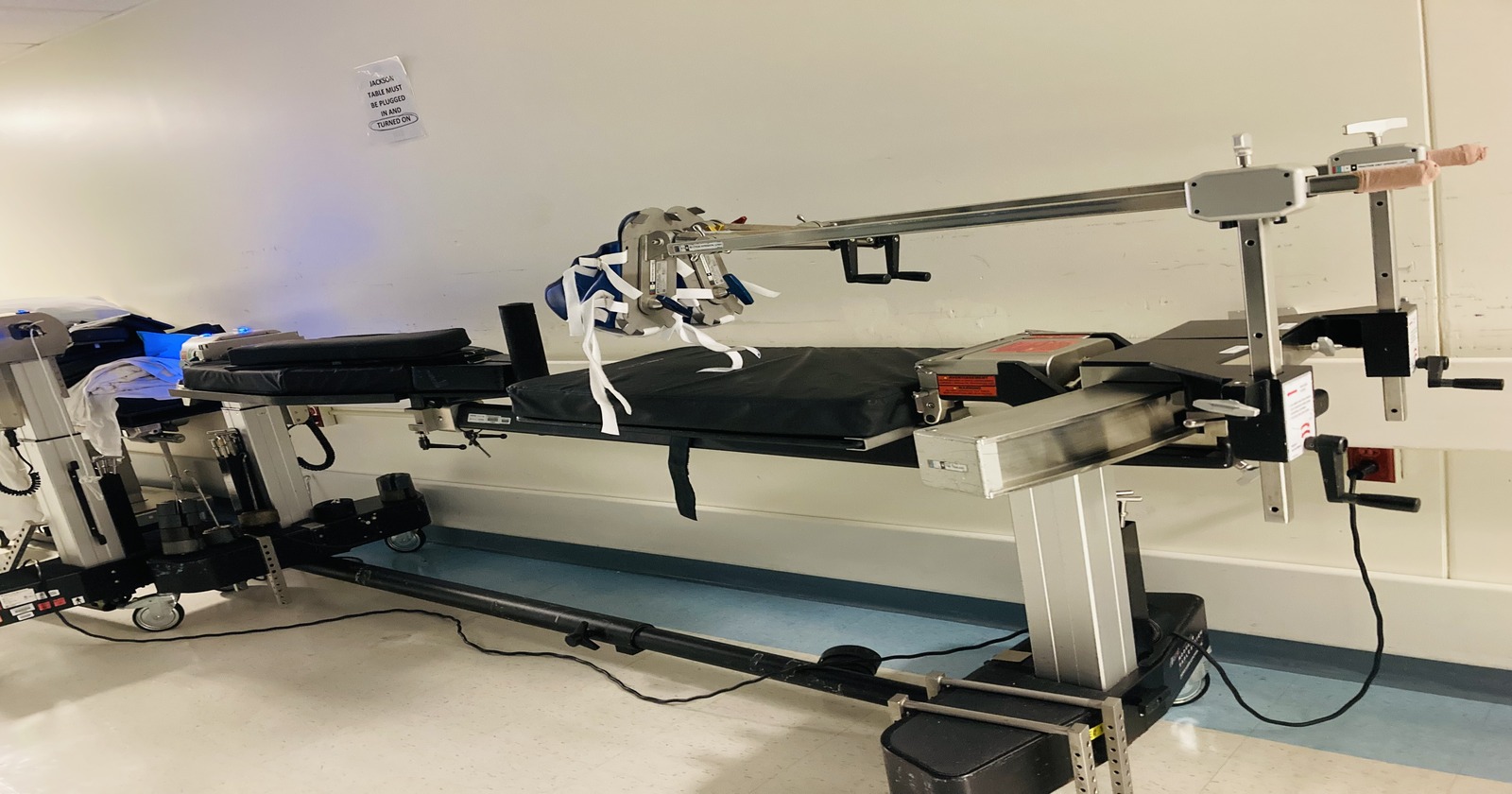
The Jackson Table is a specialized operating room table designed for spinal surgeries and procedures where precise positioning of the patient is crucial.
Orthopedic surgeons often face the decision between utilizing the Jackson Table or the Wilson Frame for positioning patients during spinal surgeries.
Understanding the distinctive features and applications of these two devices is essential for making informed choices that align with specific surgical requirements.
In this realm of orthopedic surgery, the choice between the Jackson Table and the Wilson Frame plays a significant role in achieving successful surgical outcomes. These two positioning devices offer distinct benefits and considerations, making it crucial for surgical teams to weigh their merits based on the specific needs of each procedure.
Prone Jackson (with Mayfield head clamp)

Wilson Frame

List of Differences between the Jackson table and the Wilson frame
1. The Jackson table is a specific operating room bed while the Wilson frame is just an extra Attachment for the surgical bed.
2. The Jackson table Has many Functions, for example it can do a full rotational flip from supine to prone while the Wilson frame cannot perform a rotational flip.
3. The Jackson Table can carry a patient supine, prone ,lateral or Trendelenburg while a Wilson frame is only design for prone Position.
4. The Jackson table is ideal for longer procedures with patient in prone position while the Wilson frame is for shorter procedure.
5. The Jackson table can accommodate patients with higher BMI while the Wilson frame is not recommend for heavier patients.
What is Jackson operating room table?
The Jackson table was developed by Dr. Crawford W. Long in the mid-20th century, specifically to facilitate spinal surgeries. Here are some key features and information about the Jackson Table.
The versatility of the Jackson Table lies in its modular design, which allows the use of a single base with three interchangeable tops tailored for a wide range of surgical procedures and services.
The frame supports a variety of procedures including; Orthopedic Fracture ,Trauma, Pelvic Reconstruction, Orthopedic and Neuro-Spine, Pain Management, and general procedures.
The Advanced Control Modular base of the Jackson table can hold three different tops including; the Spinal Surgery Top, Radiolucent Imaging Top, and the Orthopedic Trauma Top. Attached to the Advanced control base, the Spinal Surgery top, provides exceptional C-arm and O-arm access and is capable of bearing up to 500 pounds. It has a unique design that allows the surgeon to rotate the patient safely about the horizontal axis.
The rotational capability provides many unique advantages including specific imaging techniques. It allows the ability to perform a 360-degree rotation without removing the patient from the Jackson table, combining the anterior and posterior positioning during a single operating room visit.
The 180-degree patient rotation sequence on the Jackson table is designed to allow a patient to be rotated completely from the supine to the prone position or visa versa. Make sure to read the positioning sequence described in your operator’s manual to do this safely. In most instances, the patient will be repositioned for posterior spine surgery after the anterior spine surgery has been completed.
- Purpose: The primary purpose of the Jackson Table is to provide optimal access to the spine during surgical procedures. It allows for precise positioning, including flexion, extension, lateral bending, and rotation of the spine.
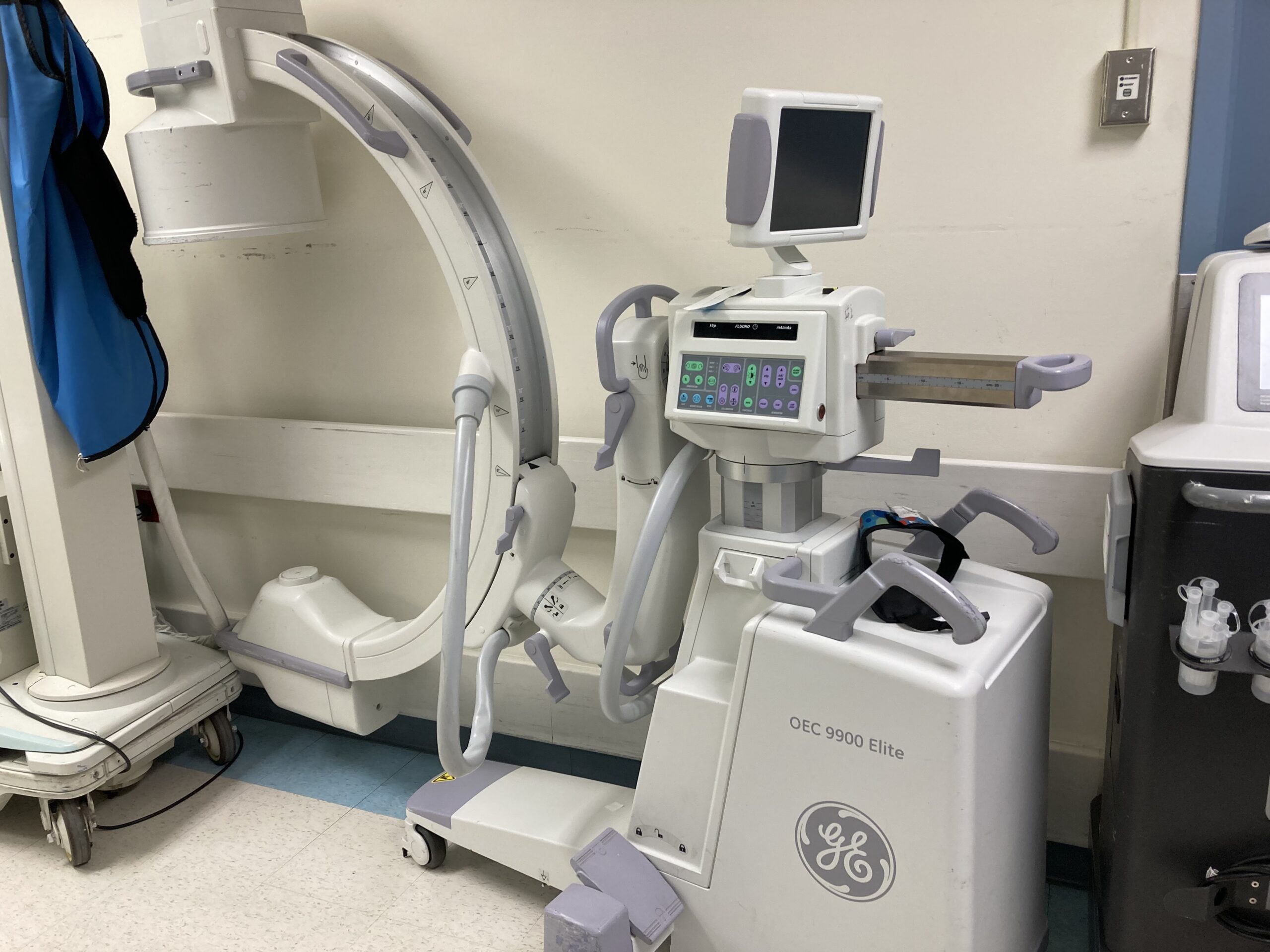
- Design: The table is characterized by its radiolucent (transparent to X-rays) surface, which allows for intraoperative imaging without the need to reposition the patient. The table itself is often constructed from carbon fiber or similar materials.
- Articulation: One of the notable features of the Jackson Table is its ability to articulate or adjust in various ways. This includes adjustments in height, tilt, and lateral tilt, which allows surgeons to achieve the desired position for the patient.
- Padding and Restraints: It often comes with specialized pads and restraints to secure the patient in the desired position while ensuring their safety and comfort during surgery.
- Application: The Jackson Table is particularly favored in procedures like spinal fusions, laminectomies, and other types of spinal surgery where precise access and alignment are critical. It is especially useful for surgeries that require extensive access to the spine.
Role of the Jackson table in Spine Surgery
Ever wondered how surgeons keep patients safe and comfortable during spinal surgeries?
Proper positioning in surgeries, especially in spinal procedures, is crucial for several reasons:
Patient Safety
- Preventing Pressure Injuries: Proper positioning helps in preventing pressure ulcers or bedsores, which can occur when a patient’s body weight is not evenly distributed.
- Avoiding Nerve Damage: Incorrect positioning can lead to nerve compression, causing temporary or permanent nerve damage. Ensuring the patient is correctly positioned minimizes the risk of such complications.
- Maintaining Circulation: Proper positioning ensures that blood flow is not impeded, which is essential for maintaining adequate tissue perfusion and preventing complications such as deep vein thrombosis.
Surgical Access
- Optimal Exposure: Correct positioning provides the surgeon with the best possible access to the surgical site. This is particularly important in spinal surgeries where visibility and access to specific vertebrae or discs are crucial.
- Stability and Control: Secure positioning keeps the patient stable and minimizes movement, allowing the surgeon to perform delicate procedures with greater precision.
- Reduction of Strain: Proper positioning can reduce the physical strain on both the patient and the surgical team, improving the overall efficiency of the procedure.
Optimal Outcomes
- Enhanced Accuracy: With the patient properly positioned, the surgeon can operate with greater accuracy, leading to better surgical outcomes.
- Shortened Surgery Time: Good positioning can lead to a more efficient surgical process, reducing the time the patient is under anesthesia, which in turn reduces the risks associated with prolonged anesthesia exposure.
- Improved Recovery: Proper positioning can contribute to less post-operative pain and a quicker recovery, as it helps in maintaining the integrity of the surgical site and preventing complications.
Proper positioning Devices such as the jackson table, in spinal surgeries is essential for ensuring patient safety, providing optimal surgical access, and achieving the best possible outcomes. It involves a meticulous approach to avoid complications and enhance the overall efficiency and success of the procedure.
7 Advantages of Jackson table
1. Precise Positioning: The table allows for highly accurate positioning of the patient’s spine, which is crucial for the success of many spinal procedures. Its also allows for precise and accurate positioning for hip, pelvic and thigh leg Orthopedic Fracture surgery.

2. Reduced Need for Repositioning: Due to its flexibility, the Jackson Table often reduces the need for repositioning during surgery, which can save time and reduce the risk of complications.
3. Optimal surgical positioning: The Jackson table allows for precise patient positioning, including flexion, extension, lateral tilt, and rotation. Surgeons can adjust the table to achieve the optimal position for accessing the surgical site, improving visibility and surgical access.
4. Reduced risk of complications: By providing stable and secure positioning during surgery, the Jackson table helps reduce the risk of complications such as nerve damage, pressure ulcers, and musculoskeletal injuries. Proper positioning also facilitates better blood circulation, which can aid in preventing intraoperative complications.
5. Enhanced surgical efficiency: The versatility of the Jackson table enables surgeons to perform complex procedures with greater efficiency.
With the ability to easily adjust patient positioning during surgery, surgeons can maintain optimal exposure of the surgical site without the need for manual repositioning or multiple table changes, saving time and improving workflow.
6. Improved patient safety and comfort: The Jackson table is designed to provide maximum patient safety and comfort during surgery. Its cushioned surface helps distribute pressure evenly, reducing the risk of pressure ulcers and discomfort during prolonged procedures. Additionally, the secure positioning offered by the table minimizes the risk of patient movement or instability during surgery.
7. Facilitates minimally invasive techniques: The Jackson table is compatible with various minimally invasive surgical techniques, such as endoscopic spine surgery and laparoscopic procedures.
Its adjustable features allow surgeons to achieve the optimal positioning required for performing these advanced techniques with precision and accuracy, resulting in better outcomes for patients.
Key Consideration when using the Jackson Table
- Cost: Jackson Tables are specialized equipment and can be relatively expensive compared to standard surgical tables.
Patient Safety
- Positioning: Ensure the patient is correctly positioned to avoid pressure sores and nerve damage. Proper alignment is critical for both patient safety and surgical outcomes.
- Padding and Support: Use adequate padding and support to protect bony prominences and soft tissues. This helps prevent pressure ulcers and nerve injuries.
- Securing the Patient: Secure the patient properly to prevent movement during the procedure, which can be critical for maintaining surgical accuracy and avoiding injuries.
Surgical Access
- Flexibility: The Jackson table allows for various positioning options (prone, supine, lateral) to provide optimal surgical access. Adjust the table as needed to facilitate the surgeon’s needs.
- Stability: Ensure the table is stable and locked in position once adjusted to prevent any unintended movements during surgery.
Anesthesia Considerations
- Airway Management: Consider the patient’s airway management, especially in prone positioning. Ensure that anesthesia providers have access to the airway and can monitor the patient effectively.
- Monitoring: Ensure that all vital signs are continuously monitored and that anesthesia equipment is accessible and functional from the position.
Equipment Compatibility
- Instrument Access: Make sure the table’s design allows for the necessary surgical instruments and imaging equipment to be used without obstruction.
- Radiolucency: The table should be radiolucent to facilitate intraoperative imaging, such as X-rays or fluoroscopy, without needing to reposition the patient.
Ergonomics
- Surgeon Comfort: Adjust the table to a height and position that is comfortable for the surgical team to minimize fatigue and improve precision.
- Staff Training: Ensure all operating room staff are trained in the use and adjustment of the Jackson table to prevent errors and enhance efficiency.
Infection Control
- Cleanliness: Maintain strict aseptic techniques to prevent infections. The table should be thoroughly cleaned and disinfected between uses.
- Draping: Proper draping techniques should be used to create a sterile field and prevent contamination.
Emergency Protocols
- Rapid Access: Ensure that there are protocols in place for rapid repositioning or emergency access if a complication arises during surgery.
- Communication: Maintain clear communication among the surgical team to quickly address any issues related to patient positioning or table adjustments.
Key parts of the Jackson table.
- Mayfield head clamp, use in some cervical spine surgery and craniotomy.

Mayfield head clamp attach to Jackson bed

Mayfield head clamp attach to prone Jackson bed
- positioning kit with padding and prone foam face pillow.
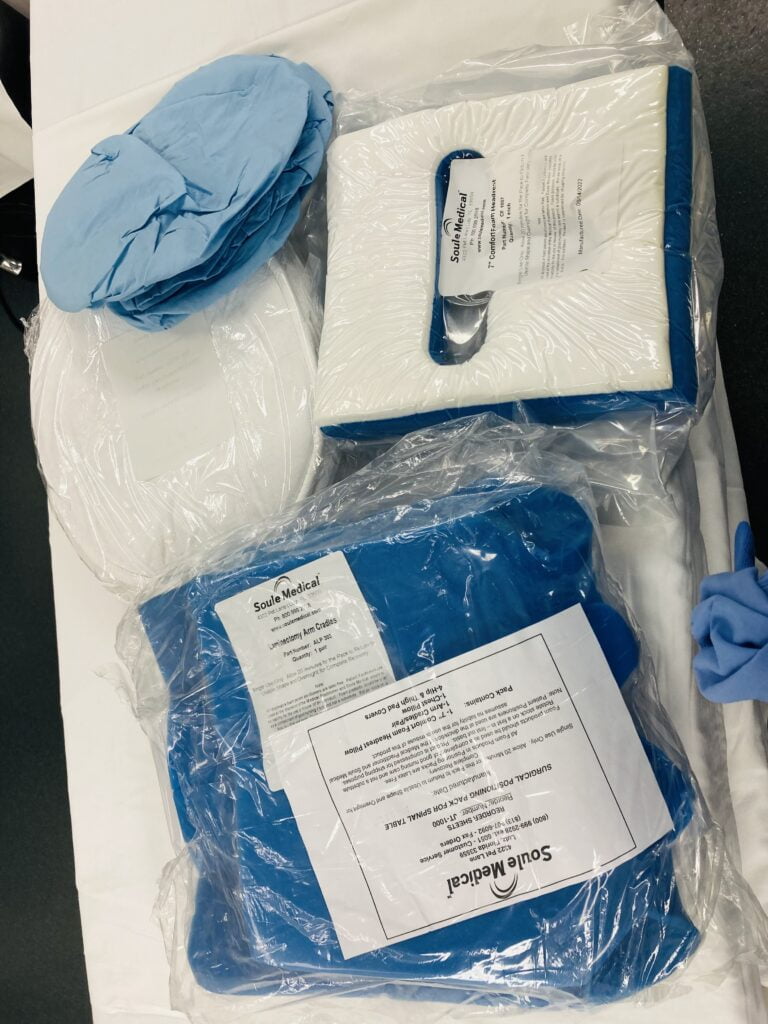
prone Jackson table kit.
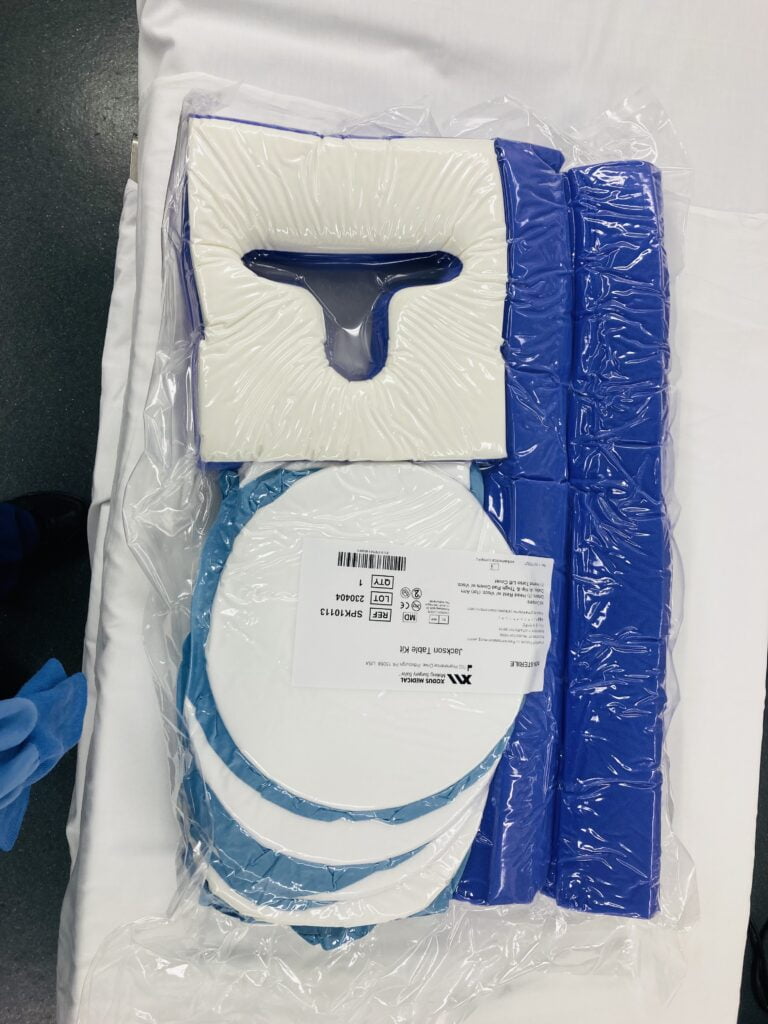
Jackson table foam face pillow hip and arm padding
- attachable H-frame.
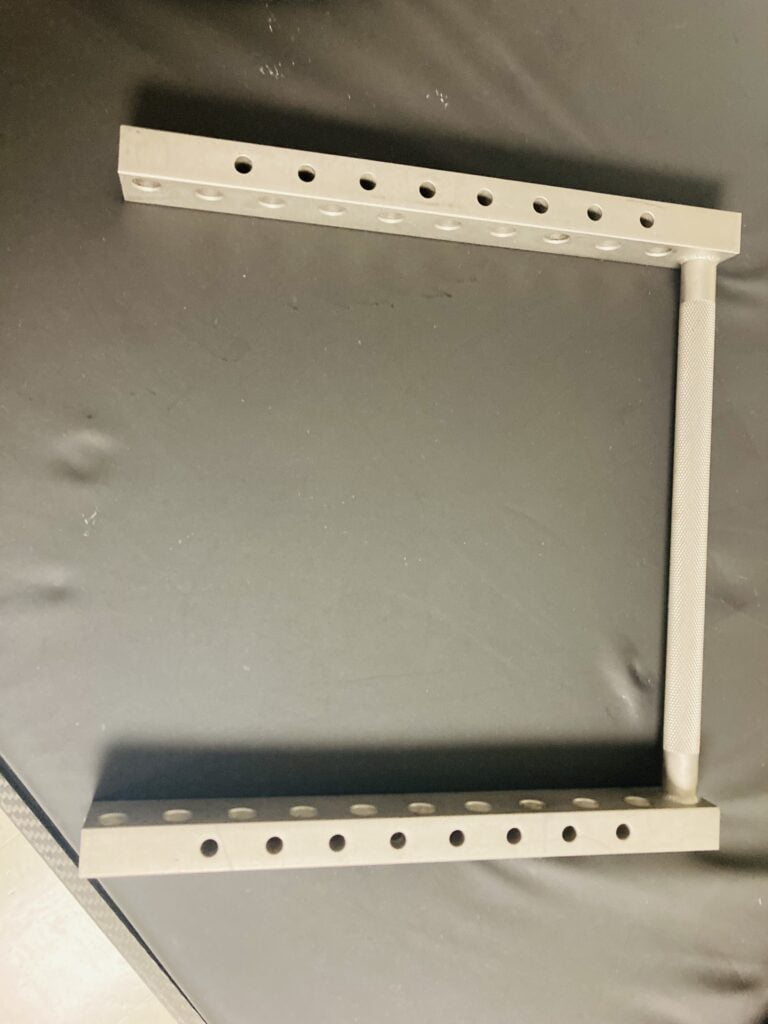
H-FRAME
- Hand and arm surgery attachment.
- Rotation and Tilting Mechanisms: Allow the table to be adjusted for different angles and positions.
- Traction unit: Used to apply gentle pulling forces to align the spine properly during surgery.
Jackson with leg attachment Traction unit
- Radiolucent Wilson frame attachment.

above photo Jackson with radiolucent Wilson frame.
- Rotatable Arm rest attachments
- Thigh and hip paddings


Control Panel: Used by the surgical team to make adjustments during the procedure.
Essential safety guidelines performing a 360 rotational flip on a Jackson table
Professional Supervision: Ensure the procedure is performed by a trained and experienced professional who is knowledgeable in using the Jackson table.
Patient Assessment: Thoroughly assess the patient’s condition to determine if they are a suitable candidate for the procedure. Consider factors like overall health, specific medical conditions, and physical limitations.
Equipment Inspection: Check the Jackson table and all associated equipment for proper function and integrity before the procedure. Ensure all components are secure and operational.
Proper Positioning: Securely and correctly position the patient on the table. Use all provided restraints and supports to stabilize the patient and prevent unintended movement during the flip.
Communication: Maintain clear communication among all team members involved in the procedure. Assign specific roles and ensure everyone understands the step-by-step process.
Slow and Controlled Movements: Perform the rotational flip slowly and in a controlled manner. Avoid sudden or jerky movements to prevent patient injury and equipment malfunction.
Monitor Vital Signs: Continuously monitor the patient’s vital signs throughout the procedure. Be prepared to stop immediately if any signs of distress or instability are observed.
Emergency Protocols: Have emergency protocols in place and ensure all team members are familiar with them. Be ready to respond quickly to any unexpected complications.
Patient Comfort: Ensure the patient’s comfort throughout the procedure. Regularly check in with the patient to address any concerns or discomfort they may experience.
Positioning the Patient:
- Initial Position: Position the patient supine (face-up) on the table.

- Padding and Supports: Place appropriate padding under pressure points to prevent injury. Use gel pads or foam pads for chest and iliac crest support (SpringerLink) (Didage).
- Securing the Patient: Secure the patient with restraints and supports, ensuring they are snug but not too tight to restrict circulation or cause discomfort (Soma Tech Intl’s Blog) (Didage).
- Arm and Leg Positioning: Place the arms either tucked at the sides or on arm boards. Legs should be padded and slightly elevated to prevent pressure sores and nerve damage (HoverTech International).
What is the Wilson Frame?
Wilson Frame on a regular O.R bed


A Wilson frame, also known as a Wilson bed or Wilson surgical bed, is a specialized piece of medical equipment used in orthopedic and surgical settings. It is named after the American orthopedic surgeon William Wilson.
The Wilson frame is designed to provide support and stabilization for patients during certain surgical procedures, particularly those involving the lower limbs, pelvis, or spine. It consists of a sturdy metal frame with adjustable components to accommodate various positions and angles needed for specific surgical techniques.
Key features of a Wilson frame may include:
- Adjustable Sections: The frame typically has adjustable sections, allowing for modifications in height, angle, and position to meet the requirements of the surgical procedure.
- Padding and Straps: The surface of the frame is usually padded to enhance patient comfort. Additionally, it may have straps or restraints to secure the patient in place during the surgery.
- Radiolucent Properties: Some modern Wilson frames are designed to be radiolucent, meaning they do not interfere with X-ray imaging. This feature is important for intraoperative imaging guidance.
- Mobility and Stability: It may have wheels for easy transportation within the operating room, and brakes to secure it in place during surgery.
- Attachment Points: The frame may have attachment points for various surgical instruments or accessories.
- Transportable : it can be easily remove from one operating room bed to another and also has an attachment for the Jackson table where it can be easily set up on the Jackson table for use.
Common uses of a Wilson frame include:
- Orthopedic Procedures: Especially those involving the hip, pelvis, or lower spine.
- Neurosurgery: For certain spinal procedures where precise positioning is critical.
- Trauma Surgery: Particularly in cases of severe fractures or dislocations.
- Plastic and Reconstructive Surgery: In procedures that require a specific positioning of limbs or body parts.
- Vascular Surgery: For procedures that require access to the lower extremities.
It’s important to note that the design and features of a Wilson frame may vary depending on the manufacturer and the specific model. Surgeons and their teams are typically trained on the proper use of this equipment to ensure patient safety and the success of the surgical procedure.
Advantages of using the Wilson frame
The Wilson frame is a medical device used in orthopedics for the management of certain types of fractures, particularly those involving the femur (thigh bone). Here are some advantages of using the Wilson frame:
- Stability: The Wilson frame provides excellent stability for patients with femoral fractures. It helps immobilize the affected leg, reducing the risk of further damage and allowing for proper healing.
- Reduces Pain: By immobilizing the fractured limb, the Wilson frame helps to minimize pain and discomfort experienced by the patient. This is crucial for patient comfort and the ability to perform daily activities.
- Early Mobilization: The frame allows for controlled weight-bearing, which means that patients can start moving around sooner than if they were immobilized in a traditional cast. This early mobilization can help prevent complications associated with prolonged bed rest.

- Minimizes Pressure Sores: Patients who are immobile for extended periods are at risk of developing pressure sores. The Wilson frame allows for repositioning and movement, reducing the likelihood of pressure ulcers.
- Adjustability: The frame is designed to be adjustable to accommodate different patient sizes and anatomies. This customization helps ensure a snug and secure fit, optimizing the support provided.
- Facilitates Rehabilitation: Physical therapy and rehabilitation are essential components of recovery from a fracture. The Wilson frame allows for easier access and participation in rehabilitation exercises, helping patients regain strength and mobility.
- Allows for Inspection and Care of Wounds: The design of the Wilson frame allows medical professionals to easily access and inspect the surgical site or wounds. This is crucial for monitoring healing progress and preventing complications.
- Can be Used in Various Positions: The Wilson frame can be adjusted to accommodate different positions, such as sitting or lying down. This versatility allows patients some degree of comfort and functionality in various situations.
- Reduces the Risk of Complications: By providing stable support, the Wilson frame can help reduce the risk of complications associated with poorly managed fractures, such as malunion, nonunion, or secondary displacement.
- Patient Comfort and Satisfaction: While any orthopedic device can be initially uncomfortable, the Wilson frame generally provides good comfort for patients compared to other forms of immobilization, particularly for long-term use.
It’s important to note that while the Wilson frame offers several advantages, its use is indicated for specific types of fractures and patient conditions. The decision to use a Wilson frame should be made by a qualified orthopedic surgeon based on the individual patient’s situation.
Please consult with a medical professional or equipment specialist for the most current and specific information about a Wilson frame, as designs and technologies in the medical field may evolve over time.
Limitations of Jackson table
- Specialized Use: The Jackson table is primarily designed for spinal surgery. It may not be suitable for other types of surgical procedures, which means that hospitals may need to invest in additional operating tables for different types of surgeries.
- Positioning Constraints: While the Jackson table is designed to provide a variety of positions for spinal surgery, it may not be as versatile for other types of procedures that require different positioning, such as cardiac or abdominal surgeries.
- Size and Space Requirements: Jackson tables tend to be large and require a significant amount of space in the operating room. This can be a limitation in smaller or more crowded surgical suites.
- Cost: Jackson tables are specialized equipment and can be expensive to purchase and maintain. Hospitals may need to carefully consider the budgetary implications of acquiring and maintaining this equipment.
- Learning Curve: Properly using a Jackson table requires training and expertise. Surgeons and operating room staff need to be familiar with the table’s features and functions to use it effectively and safely.
- Patient Weight and Size Limitations: Some models of Jackson tables may have weight and size limitations, which could restrict their use for certain patients.
- Maintenance and Repairs: Like any piece of medical equipment, Jackson tables require regular maintenance and occasional repairs. This can add to the overall cost of ownership.
- Accessibility and Transfer: Getting a patient onto and off of a Jackson table may be more challenging for certain patients, especially those with mobility issues or other medical conditions.
- Availability and Backup: If a hospital only has one Jackson table and it requires maintenance or is in use for another procedure, this could potentially lead to scheduling conflicts and delays in surgical procedures.
- Limited Applicability in Non-Spinal Procedures: While the Jackson table is excellent for spinal surgeries, it may not be the best choice for surgeries that involve other body systems.
- Robotic and Laparoscopic Surgery: Cannot be use for a Robotic procedure or a laparoscopic procedure.
Disadvantages of the Wilson Frame
- Limited Mobility: Patients placed in a Wilson frame generally have restricted mobility. This can be uncomfortable and frustrating for patients, and it can lead to complications such as pressure sores and muscle atrophy if used for extended periods.
- Not Suitable for All Patients: The use of a Wilson frame is typically limited to patients who meet specific criteria. It may not be appropriate for patients with certain medical conditions, such as those with unstable fractures or severe respiratory issues.
- Pressure Sores: Prolonged use of a Wilson frame can increase the risk of pressure sores, especially if the patient is unable to change positions or receive regular repositioning.
- Dependency on Caregivers: Patients in a Wilson frame often require significant assistance from caregivers or healthcare professionals for activities of daily living, including bathing, toileting, and feeding. This can increase the workload on healthcare staff.

- Psychological Impact: Prolonged confinement to a Wilson frame can lead to psychological stress and discomfort for patients, potentially affecting their overall well-being.
- Limited Use for Certain Conditions: While Wilson frames are useful for managing specific orthopedic conditions or post-operative care, they are not a universal solution and may not address the needs of patients with other medical conditions.
- Incompatibility with Some Treatments: Certain treatments or therapies may not be feasible or effective for patients in a Wilson frame, which can limit the range of care options.
- Transfer and Mobility Challenges: Moving patients in and out of a Wilson frame can be challenging, requiring specialized equipment and trained personnel. This can pose logistical difficulties in a healthcare setting.
- Potential Complications: If not used properly or if the patient’s condition changes, complications such as joint contractures, muscle weakness, or pneumonia may arise.
- Impact on Daily Activities: Patients in a Wilson frame may have limited ability to engage in daily activities and participate in rehabilitation exercises, potentially slowing down the recovery process.
- Patient discomfort and immobility: While the Wilson frame provides stability, it can also be uncomfortable for the patient, particularly during prolonged use. Immobilization for an extended period can lead to muscle atrophy, joint stiffness, and overall discomfort for the patient.
- Limited access for wound care: The design of the Wilson frame can restrict access to the injured area, making it difficult to perform necessary wound care or surgical procedures. This limitation can hinder the management of complications that may arise during the healing process.
- Difficulty in transportation: The bulky nature of the Wilson frame can make transportation of the patient challenging. It may require specialized equipment or additional assistance to move the patient safely, particularly in settings such as ambulances or helicopters.
It’s essential for healthcare providers to carefully assess each patient’s condition and needs before using a Wilson frame. While it can be a valuable tool for specific medical situations, its limitations should be taken into account to ensure that it is used appropriately and that patients receive the best possible care. Additionally, healthcare professionals should monitor patients in Wilson frames closely to address any potential complications or discomfort promptly.
Weight limit of the Jackson table and the Wilson Frame
The weight capacity of a Jackson table ranges from 350 to 500 pounds (159 to 227 kilograms), depending on the specific model and manufacturer.

The Wilson frame, often used in conjunction with a surgical table for positioning patients during spinal and other procedures, also has specific weight limits. The typical weight capacity for a Wilson frame is around 250 to 350 pounds (113 to 159 kilograms), but this can vary based on the manufacturer and model.https://www.mizuhosi.com/product/wilson-plus-radiolucent-lumbar-frame/
Common questions about the Jackson table and Wilson frame, with answers for each:
General Questions
1. What are the Jackson table and Wilson frame used for?
- The Jackson table and Wilson frame are used to position patients during spinal surgeries. They help ensure optimal access for the surgeon and maintain the patient’s safety and comfort.
2. Why is proper positioning important in spinal surgeries?
- Proper positioning is crucial in spinal surgeries to ensure the surgeon has the best access to the surgical site, to minimize the risk of pressure injuries, and to maintain the patient’s physiological stability throughout the procedure.
3. What are the differences between the Jackson table and Wilson frame?
- The Jackson table is a complex, adjustable table designed for a variety of surgical positions, offering versatility and stability. The Wilson frame, on the other hand, is a simpler device primarily used to support the patient’s torso in a flexed position, ideal for certain types of spinal surgeries.
Specific Questions About the Jackson Table
1. How does the Jackson table work?
- The Jackson table consists of a radiolucent platform that can be adjusted to various angles and positions. It allows for the patient to be positioned prone, supine, or lateral, making it versatile for different surgical needs.
2. What are the main features of the Jackson table?
- Key features include radiolucent materials for clear imaging, adjustable sections for precise positioning, and support structures to ensure patient stability and safety.
3. Why would a surgeon choose a Jackson table over other positioning devices?
- A surgeon might choose a Jackson table for its versatility, especially for complex or lengthy surgeries that require multiple positioning adjustments or clear imaging.
4. Are there any risks or downsides to using the Jackson table?
- While generally safe, potential risks include the complexity of setup and adjustments, which require thorough training to avoid positioning errors that could lead to patient discomfort or pressure injuries.
Specific Questions About the Wilson Frame
1. How does the Wilson frame work?
- The Wilson frame is placed on a standard operating table and supports the patient’s torso in a flexed position, which is often required for lumbar spinal surgeries.
2. What are the main features of the Wilson frame?
- It includes adjustable pads to fit various body sizes and shapes, and it allows for controlled flexion of the spine to improve surgical access and reduce intra-abdominal pressure.
3. In what types of surgeries is the Wilson frame most commonly used?
- The Wilson frame is commonly used in lumbar spinal surgeries, such as laminectomies and discectomies, where a flexed position is beneficial.
4. Are there any risks or downsides to using the Wilson frame?
- Risks include the potential for pressure sores if not properly cushioned, and it may not provide the stability needed for more complex surgeries.
Patient-Centered Questions
1. How does the choice of positioning device affect the patient’s experience and recovery?
- The right positioning device can minimize intraoperative complications and postoperative discomfort, leading to a smoother recovery process.
2. Is one device more comfortable for patients than the other?
- Comfort can vary based on the surgery type and duration. The Jackson table may offer more comfort for longer, complex surgeries due to its adjustability, while the Wilson frame is effective for shorter, specific procedures.
3. Can the use of these devices impact the success rate of surgeries?
- Yes, proper positioning can enhance surgical access and precision, potentially improving the success rates and reducing complications.
Technical and Practical Questions
1. How are these devices cleaned and maintained?
- Both devices require regular cleaning and maintenance according to manufacturer guidelines, involving disinfection of surfaces and inspection of mechanical parts to ensure proper functioning.
2. What kind of training do medical staff need to use these devices properly?
- Medical staff need specialized training to understand the setup, adjustments, and safety precautions associated with each device to ensure patient safety and optimal positioning.
3. Are there any new advancements in surgical positioning technology?
- Yes, advancements include automated positioning systems, enhanced imaging compatibility, and improved ergonomics for both patients and surgical teams.
Cost and Accessibility Questions
1. How much do these devices cost?
- The cost can vary widely; the Jackson table is typically more expensive due to its complexity and versatility, while the Wilson frame is relatively less costly.
2. Are there cost-effective alternatives to the Jackson table and Wilson frame?
- Yes, there are simpler positioning devices available, but they may not offer the same level of functionality and safety features.
3. Are these devices available in all hospitals, or only specialized centers?
- These devices are more commonly found in specialized surgical centers and hospitals with a high volume of spinal surgeries.
Safety and Efficacy Questions
1. Are there any safety concerns with using the Jackson table or Wilson frame?
- Safety concerns include ensuring proper setup and adjustment to prevent pressure injuries and ensuring the devices are regularly maintained to avoid mechanical failures.
2. How do these devices improve the safety and efficacy of spinal surgeries?
- They enhance surgical access, minimize patient movement, and reduce the risk of pressure-related injuries, contributing to safer and more effective surgeries.
3. What do studies say about the outcomes of surgeries using these devices?
- Studies generally support the efficacy and safety of both devices, highlighting improved surgical outcomes and reduced complications when used properly.
Visual and Practical Demonstration Questions
1. Can you show a video or demonstration of these devices in use?
- Yes, many manufacturers and medical education platforms offer videos demonstrating the setup and use of these devices.
2. What does the setup process look like for each device?
- The Jackson table setup involves adjusting various sections for the specific surgical procedure, while the Wilson frame involves positioning and securing it on a standard table and adjusting the pads for patient comfort.
3. How do surgeons and operating room staff prepare the devices before surgery?
- Preparation includes thorough cleaning, proper positioning adjustments, and ensuring all safety features are in place before the patient is positioned.
Future and Innovation Questions
1. What are the latest innovations in surgical positioning devices?
- Innovations include integration with robotic surgery systems, enhanced imaging compatibility, and automated adjustment features to improve precision and ease of use.
2. How might future technology improve upon the Jackson table and Wilson frame?
- Future technologies may offer more precise and automated adjustments, better patient monitoring during surgery, and improved ergonomic designs for both patients and surgical teams.
3. Are there any upcoming devices that might replace these in the future?
- While new devices are continually being developed, the Jackson table and Wilson frame remain standards in many procedures due to their proven efficacy. Future replacements will likely build on their strengths with enhanced features.
Recovery and Post-Surgery Questions
1. How do these devices impact post-surgery recovery times?
- Proper positioning can reduce intraoperative trauma and postoperative pain, potentially leading to faster recovery times.
2. Are there any special considerations for patients positioned on these devices during surgery?
- Special considerations include monitoring for pressure sores, ensuring proper support, and careful repositioning during longer surgeries to maintain patient comfort and safety.
Addressing patients Common Concerns
1. What should patients know about their positioning during surgery?
- Patients should understand that proper positioning is crucial for the success of the surgery and that their surgical team is trained to ensure their safety and comfort.
2. How can patients ensure they are getting the best possible care when it comes to surgical positioning?
- Patients can discuss with their surgeons the type of positioning device that will be used and the measures taken to ensure their safety and comfort during the procedure.
Disclaimer
The information provided in this article is for educational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or medical equipment. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Resources
Work experiences , on the job training, images was taken by author while working with the medical devices.