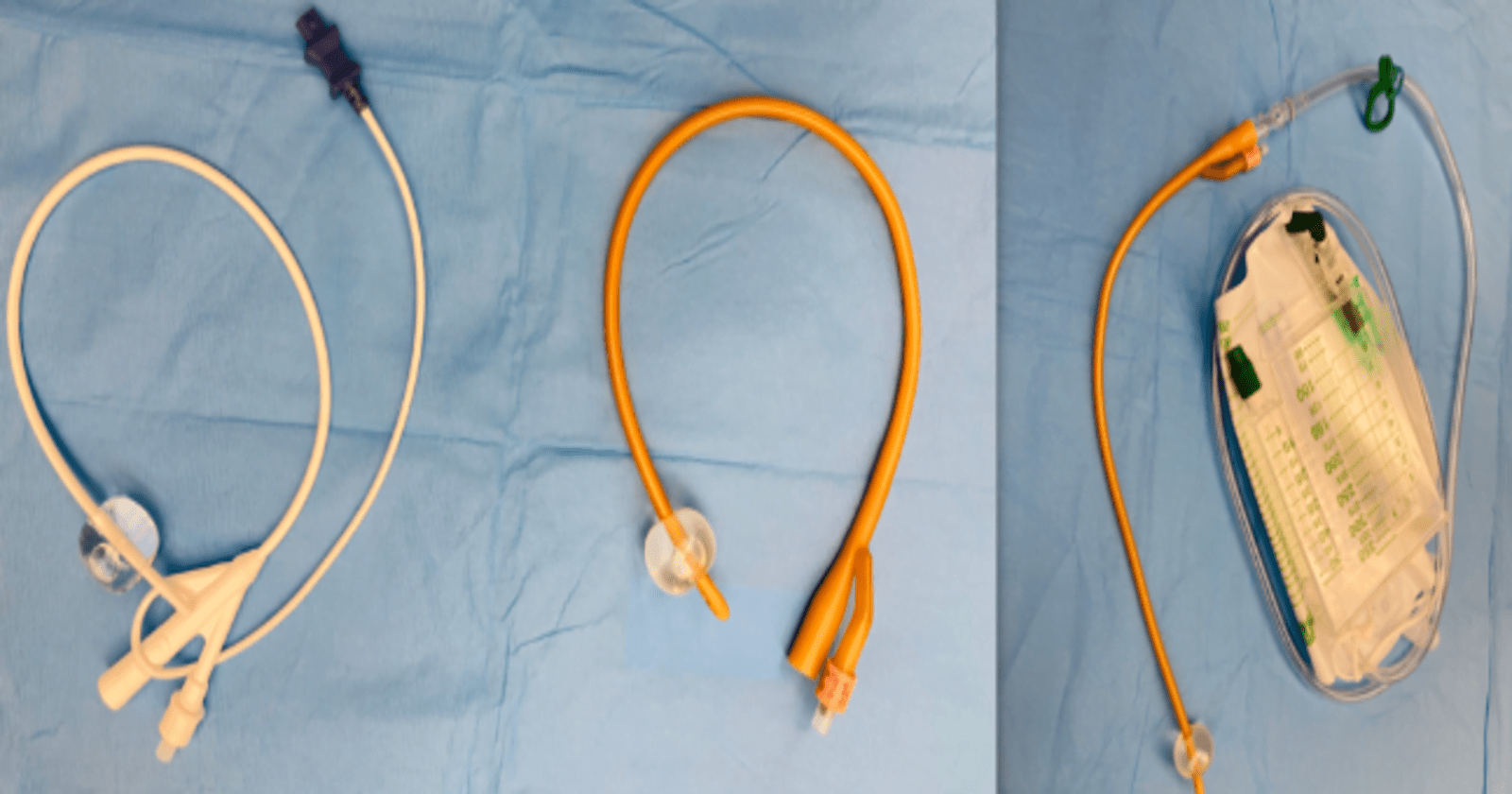
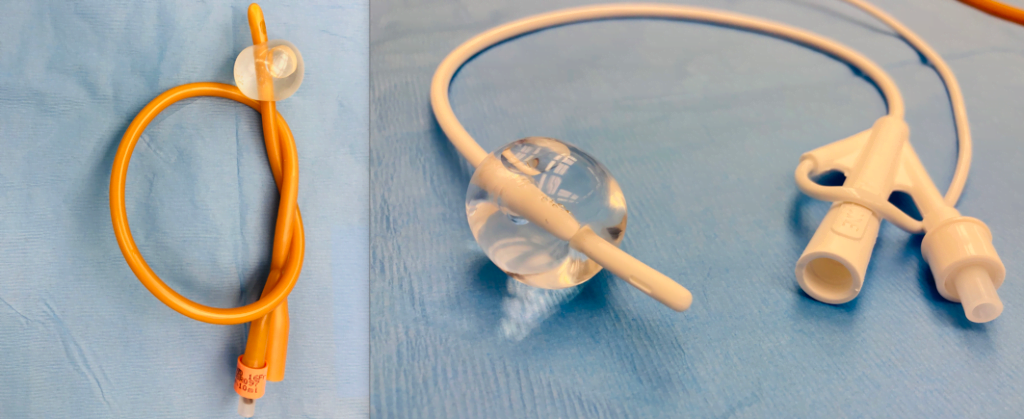
Indwelling Foley catheters and supra-pubic catheters are medical devices employed to facilitate the drainage of urine from the bladder. The Foley catheter is a flexible tube inserted through the urethra into the bladder, secured by a small inflatable balloon.
This catheter is typically used for short-term urinary drainage. Conversely, the suprapubic catheter is inserted through a small incision in the lower abdomen directly into the bladder, making it suitable for long-term use.
| Foley Catheter | Suprapubic Catheter |
|---|---|
| Inserted through the urethra into the bladder | Inserted directly into the bladder through the abdominal wall |
| Supine position, legs slightly apart | Supine position, often with mild sedation or local anesthesia |
| Cleaning of the genital area with antiseptic | Cleaning of the lower abdomen, ultrasound guidance may be used |
| Lubricated catheter inserted through the urethral opening | Small incision made above the pubic bone, catheter inserted through the incision |
| Typically, no anesthesia is used | Local anesthesia or mild sedation used |
| Discomfort is common, especially in males; burning sensation or pressure | Minimal pain due to anesthesia; may feel pressure or brief sharp pain during incision |
| Mild discomfort may persist initially | Mild soreness at the insertion site, usually subsides as healing occurs |
| Catheter held in place by inflating a balloon in the bladder | Catheter secured with sutures or adhesive device; directly into bladder through abdominal wall |
| Short to medium-term | Often used for long-term bladder management |

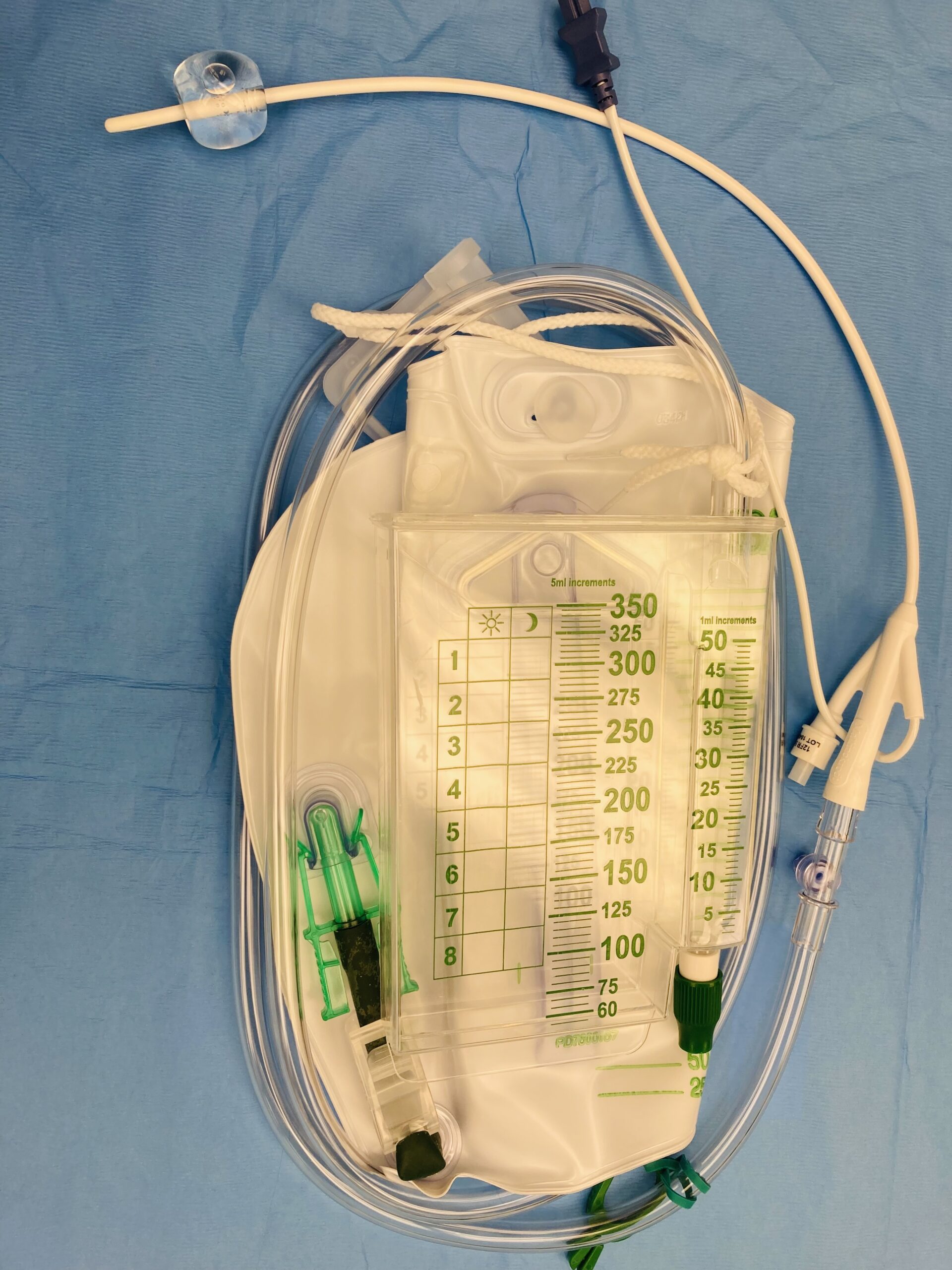
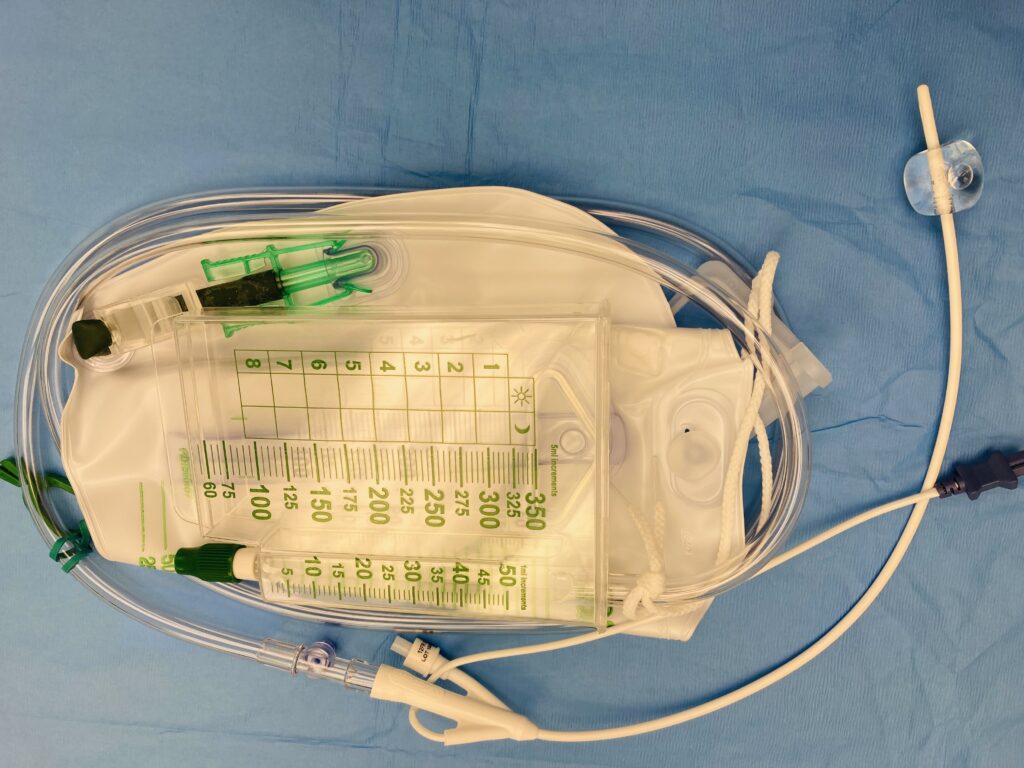
Both catheters are connected to drainage bags that collect the expelled urine. Their selection depends on factors such as the patient’s medical condition and the anticipated duration of catheterization, and should always be administered and managed by a healthcare professional to ensure proper care and minimize potential complications.

Unlocking the Secrets of Indwelling Catheters: Navigating the Intricacies with Care and Precision
A Foley catheter, named after its inventor Frederic Foley, is a type of indwelling urinary catheter. It is a flexible, hollow tube that is carefully placed into the bladder via the urethra. This catheter serves a vital purpose for individuals who, due to various factors such as undergoing surgery with anesthesia or experiencing bladder-related issues, are unable to naturally empty their bladder.
Unlike the usual process where urine accumulates in the bladder until it’s expelled during urination, the Foley catheter ensures a continuous drainage of urine from the bladder. The expelled urine is collected in a bag, which can be emptied as necessary.
The indwelling Foley catheter was invented by Dr. Frederic Foley in the early 1930s. He designed this catheter to provide a more secure and reliable method of draining urine from the bladder compared to earlier catheter designs. Dr. Foley’s innovation has since become a standard medical tool for managing urinary retention and other related conditions.
Inserting a Foley catheter involves several steps, which are carried out using sterile technique to minimize the risk of infection. Here is a list of the typical steps:
Step by Step technique for Insertion of a foley Catheter
- Gather Necessary Supplies:
- Foley catheter kit
- Sterile gloves
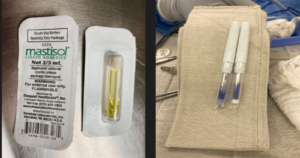
- Antiseptic solution (e.g., Betadine) .If patient has an allergy to iodine donot use betadine ,there is other options.
- Sterile drape
- Lubricating jelly at the health care , UROJET is use .Its a combination of lidocaine jelly.
- Syringe with sterile water (for balloon inflation)
- Explain the Procedure to the Patient:
- Inform the patient about the need for catheterization and reassure them that the procedure will be performed as gently as possible. Usually in the operating room we wait until anesthesia has put the patient to sleep and have it remove before they awake if there is no need to keep it post OP
- Position the Patient:
- Place the patient in a comfortable, supine position with legs slightly apart or what we call frog leg for a female patient. Male patient stay supine.
- Prepare the Area:
- Ensure privacy and drape the patient appropriately to expose the genital area. Clean the area around the urethral meatus with antiseptic solution.
- Don Sterile Gloves:
- Properly wash hands and put on sterile gloves to maintain aseptic conditions.
- Lubricate the Catheter:
- Apply a generous amount of sterile lubricating jelly to the tip and first few inches of the catheter.
- Insert the Catheter:
- Gently insert the catheter through the urethral opening until urine flows, indicating it has entered the bladder. Advance it another 2-3 inches to ensure proper placement.
- Inflate the Balloon:
- Using a syringe, inflate the balloon with the prescribed amount of sterile water. This secures the catheter in the bladder.

9. Attach the Collection Bag:
- Connect the drainage tubing to the catheter and secure it to the patient’s thigh.
10. Ensure Proper Positioning:
- Make sure the catheter is not under tension or kinked, and that it is draining properly into the collection bag.
11. Secure the Catheter:
- Attach the catheter to the patient’s leg using a securement device to prevent movement.
12. Document the Procedure:
- Record the date, time, size of the balloon inflated, and any relevant observations in the patient’s medical chart.
13. Educate the Patient:
- Inform the patient about the catheter, its purpose, and what to expect during its use.
Remember that each patient may have specific considerations or variations in their care, so it’s important to follow the protocols and guidelines established by the healthcare facility and consult with the healthcare team as needed.
Differences in Insertion and Placement of a foley catheter and a supra-pubic catheter
Foley Catheter:
- Preparation:
- The patient is placed in a supine position, with the legs slightly apart.
- The genital area is cleaned with antiseptic to minimize the risk of infection.
- Sterile gloves and equipment are used throughout the procedure.
- Insertion:
- The catheter is lubricated to ease its passage through the urethra.
- For male patients, the penis is gently held upright, and the catheter is inserted through the urethral opening. For female patients, the labia are separated, and the catheter is inserted into the urethral meatus.
- The catheter is advanced gently until urine starts to flow, indicating that it has reached the bladder.
- Once urine flow is confirmed, the balloon at the catheter tip is inflated with sterile water to keep the catheter in place.
- The catheter is then connected to a drainage bag, and the external portion is secured to the patient’s thigh or abdomen to prevent movement.
- Placement:
- The Foley catheter remains in the bladder, allowing continuous drainage of urine. The balloon prevents it from slipping out.
2. Suprapubic Catheter:
- Preparation:
- The patient is typically in a supine position, often with mild sedation or local anesthesia.
- The lower abdomen is cleaned and draped with sterile coverings.
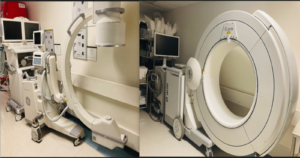
- An ultrasound may be used to guide the placement.
- Insertion:
- A small incision is made just above the pubic bone, where the bladder can be accessed directly.
- A trocar (a sharp, pointed instrument) is used to create an entry point into the bladder.
- Once the bladder is accessed, the catheter is inserted through the abdominal wall and into the bladder.
- The catheter is then secured in place with sutures or an adhesive device, and the external portion is connected to a drainage bag.
- Placement:
- The suprapubic catheter is positioned directly into the bladder through the abdominal wall. It is often used for long-term bladder management.
Pain and Discomfort Comparison
Foley Catheter:
- During Insertion:
- Discomfort during Foley catheter insertion is common, particularly for male patients due to the longer urethra. The discomfort is usually described as a burning sensation or pressure as the catheter passes through the urethra.
- Pain levels can vary, but with proper lubrication and technique, severe pain is generally avoided. Anxiety can also amplify the sensation of discomfort.
- After Insertion:
- Mild discomfort may persist initially as the body adjusts to the presence of the catheter. This discomfort typically decreases over time.
Suprapubic Catheter:
- During Insertion:
- Pain is usually minimized through the use of local anesthesia or sedation during the procedure. The initial incision and puncture of the bladder wall can cause a brief sharp pain.
- Patients may feel pressure or discomfort as the catheter is positioned, but the overall pain during insertion is often less pronounced compared to Foley catheterization due to the use of anesthesia.
- After Insertion:
- Post-procedure discomfort is generally mild but may include soreness around the insertion site. This discomfort usually subsides as the site heals. The risk of infection at the incision site can cause additional discomfort if not properly managed.
How to care for a someone with a Foley Catheter
Hand Hygiene:
Always wash your hands thoroughly with soap and water before and after handling the catheter.
Regular Observation:
Check the catheter site and the drainage bag regularly for signs of infection, irritation, or other issues.
Positioning:
Ensure that the catheter tubing is positioned in a way that it doesn’t kink or loop, which could obstruct urine flow.
Securement:
Make sure that the catheter is securely taped to the thigh or abdomen to prevent any tugging or pulling.
Maintain Bag Position:
Keep the drainage bag lower than the bladder to allow proper drainage. It should not touch the floor.
Emptying the Drainage Bag:
Drain the bag when it is half full or as instructed by a healthcare provider.
Clean the outlet valve and surrounding area with soap and water after emptying.
Cleaning the Tubing:
Clean the tubing gently with warm soapy water and rinse thoroughly.
Avoid using alcohol or harsh chemicals, as they can damage the catheter.
Peri-care (for female patients):
Clean the area around the catheter entry site with warm soapy water, wiping from front to back.
Rinse and pat dry.
Secure the Tubing:
Secure the catheter tubing with a leg strap or tape to prevent any tension or pulling.
Prevent Tension:
- Ensure that there is no tension on the catheter, especially during movement.
Hydration:
2. Encourage the patient to maintain good hydration to prevent urinary tract infections.
3. Maintain Bag Sterility: age port of the bag to touch any surfaces.
Clothing Considerations:
4. Wear loose-fitting clothing to prevent any pressure on the catheter or tubing.
Avoid Tugging or Pulling:
5. Handle the catheter gently and avoid any tugging or pulling on the tubing.
Report Any Problems:
6. If you notice signs of infection (such as fever, foul odor, or cloudy urine), bleeding, or any other issues, inform a healthcare provider immediately.
3. Remember, these are general guidelines. Always follow the specific instructions provided by a healthcare professional. If you have any concerns or questions about Foley catheter care, consult a healthcare provider for guidance.
18 Key considerations and ideas for an Indwelling Foley Catheter
1. In the context of indwelling Foley catheters, it’s important to factor in considerations such as the risk of infection.
2. Comfort and Mobility: Ensure that the catheter is positioned comfortably to allow for normal movement and activities.
3. Proper Insertion Technique: It’s crucial that the catheter is inserted using sterile techniques to minimize the risk of infection.
4. Securement: Adequate and proper securement of the catheter helps prevent movement or dislodgement.
5. Drainage System Integrity: Regularly check the catheter and drainage system for any leaks or blockages.
6. Skin Care: Proper hygiene and care of the area around the catheter site can prevent skin irritation or infection.
7. Bladder Spasms: Some individuals may experience bladder spasms, which should be managed appropriately.
8. Monitoring Output: Keep track of urine output to ensure the catheter is functioning properly and to monitor for any changes.
9. Patient Education: Educate the patient and caregivers about catheter care, signs of infection, and when to seek medical attention.
10. Regular Follow-up: Scheduled appointments with healthcare providers are important to monitor the catheter’s function and address any concerns.
11. Potential Complications: Be aware of potential complications like blockages, encrustations, and catheter-associated urinary tract infections (CAUTIs).
12. Hydration: Ensure the patient is adequately hydrated to maintain healthy urinary function.
13. Infection Prevention: Follow proper aseptic techniques during catheter care to minimize the risk of infection.
14. Patient Comfort: Address any discomfort or pain associated with the catheter promptly.
15. Alternative Methods: Consider if there are alternative methods of urinary management that might be more suitable for the patient’s long-term care.
16. Documentation: Accurate and thorough record-keeping of catheter care, including changes and observations, is crucial for continuity of care.
17. Patient Preferences and Goals: Consider the patient’s preferences and long-term goals when determining the most appropriate urinary management method.
18. Remember, these considerations should be tailored to individual patient needs and assessed by a healthcare professional with expertise in catheter care.
Supra-pubic Catheter Care: Ensuring Comfort and Best Practices
A suprapubic catheter is a medical device used to facilitate the drainage of urine from the bladder. It is inserted through a small incision in the abdomen. A healthcare provider can educate you on how to perform necessary changes and upkeep, including regular flushing to prevent blockages. Typically, you should experience improved comfort at the incision site within two weeks.
A suprapubic catheter (SPC) is a flexible tube typically made of rubber or plastic, used by healthcare providers to drain urine from the bladder when a person is unable to urinate naturally. Unlike a traditional urethral catheter, which is inserted through the urethra, an suprapubic catheter is placed through a small incision in the lower abdomen to directly access the bladder for drainage.
14 When and Why You Might Need a Suprapubic Catheter
- Urinary incontinence.
- Pelvic organ prolapse.
- Prostate cancer.
- Prostate enlargement (benign prostatic hyperplasia).
- Surgery on the prostate or genitals.
- Spinal cord injury.
- Lower body paralysis (paraplegia).
- Multiple sclerosis (MS).
- Epidural administration (temporary loss of bladder control).
- Parkinson’s disease.
- Urethral stricture.
- Inability to retract the foreskin (phimosis).
- Buried penis.
- Scarring.
Please note that the decision to use a suprapubic catheter should be made by a qualified healthcare professional based on the specific medical condition and circumstances of the individual patient.
Considerations for Supra-Pubic Catheter
- Medical Necessity: SPCs are typically recommended when there is a medical condition that prevents normal urination. This could be due to factors like urinary retention, surgery, neurological conditions, or other underlying medical issues.
- Patient Preference: In some cases, patients may have a preference for a suprapubic catheter over a urethral catheter. This preference should be taken into consideration and discussed with the patient.
- Anatomy and Physiology: An assessment of the patient’s lower abdominal anatomy is essential to determine the optimal placement site for the catheter. This is typically located about 2-3 cm above the pubic bone and slightly to one side.
- Infection Risk: The risk of infection is an important consideration. Proper sterile technique during insertion and ongoing catheter care are critical to minimize this risk.
- Skin Condition: The condition of the skin in the lower abdomen is important. It should be free of any infection, lesions, or abnormalities that could interfere with the healing process.
- Mobility and Activity Level: Consideration should be given to the patient’s level of mobility. An SPC may be preferred for patients who have limited mobility or are bedridden.
- Patient Education and Consent: It’s important to educate the patient about the procedure, the care and maintenance of the catheter, and potential complications. Informed consent should be obtained.
- Potential for Complications: The potential for complications, such as infection, leakage, or blockage, should be discussed with the patient. They should be aware of signs of complications and when to seek medical attention.
- Long-term vs. Temporary Use: The expected duration of catheter use is a crucial consideration. In some cases, an SPC may be a temporary solution while in others, it may be a long-term requirement.
- Alternatives: Other options for managing urinary issues should be considered. This may include intermittent catheterization, medications, or surgical interventions.
- Follow-up Care: Plans for ongoing care and monitoring should be established, including scheduled catheter changes, regular check-ups, and a plan for managing any complications that may arise.
Ultimately, the decision to use a suprapubic catheter should be based on a thorough assessment of the patient’s specific medical condition and needs, and should be made by a qualified healthcare professional.
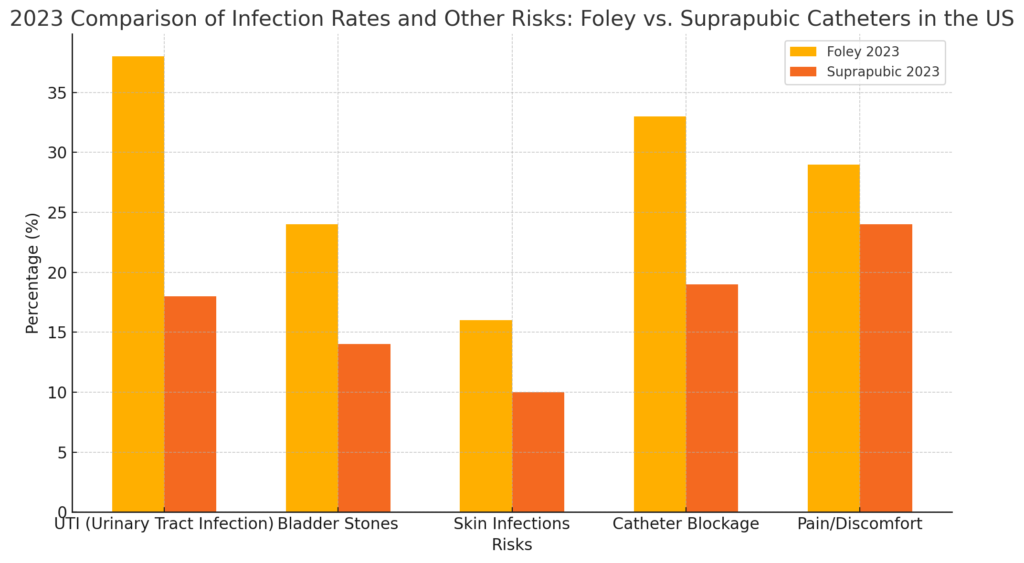
Comparison of infection rates and other risks with long-term Foley vs. suprapubic catheters.
Resources
https://www.fda.gov/media/130865/download
https://my.clevelandclinic.org/health/treatments/25028-suprapubic-catheter
Personal work experience as an R.N