Dermabond and liquid bandage are both popular choices for wound closure, each offering distinct advantages depending on the situation. Dermabond, also known as surgical glue, is a medical-grade adhesive designed for deeper, surgical wounds. It forms a strong, flexible bond that holds wound edges together, promoting efficient healing and minimizing scarring.
Dermabond is often used in situations where stitches or staples might be required, but it offers the advantage of being quicker to apply and less invasive.

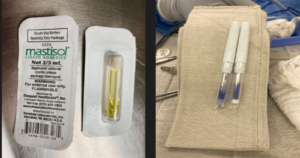
Dermabond and liquid bandage.
On the other hand, liquid bandage is a flexible, protective coating made of a polymer blend that dries rapidly upon application. It’s ideal for minor cuts, abrasions, and shallow wounds.
Liquid bandage provides a breathable, waterproof barrier that shields the wound from external contaminants while allowing the skin to breathe, aiding in the natural healing process.
While both products have their merits, the choice between Dermabond and liquid bandage ultimately depends on the type and severity of the wound, as well as the desired level of wound closure and protection.
What is Dermabond
Dermabond is a type of adhesive that relies on cyanoacrylate for its composition. It is specially designed for closing wounds on the skin. This adhesive serves as a substitute for conventional sutures or stitches in specific cases.
Dermabond offers a swift and convenient approach to seal minor cuts and lacerations. It forms a pliable, water-resistant barrier that aids in shielding the wound from potential bacterial or contaminant exposure.
Mostly use in a hospital setting ,usually for surgical wound closure.
Advantageous features of Dermabond
- Swift Application: Dermabond is swiftly applied topically, drying promptly and expediting wound closure compared to conventional sutures.

- No Removal Required: Unlike sutures or staples, Dermabond naturally sloughs off as the wound heals, eliminating the need for removal.
- Diminished Scarring: Dermabond fosters less conspicuous scarring, providing a smooth, uniform surface for optimal wound healing.
- Water-Resistant: Once fully cured, Dermabond becomes water-resistant, enabling patients to shower or bathe without concern for compromised adhesion.
- Bacterial Barrier: It forms a protective shield over the wound, mitigating the risk of infection.
- Flexibility: Dermabond is pliable and moves in tandem with the skin, especially beneficial for wounds in areas prone to movement.
- Transparent Finish: It dries to a clear finish, allowing healthcare professionals to monitor the wound without necessitating dressing removal.
- Minimal Tissue Impact: Dermabond is gentle on the skin, causing minimal tissue trauma, resulting in reduced patient discomfort.
- Precise Application: Applied in a controlled manner using a specialized applicator, Dermabond allows for accurate placement on the wound.
- Versatility: Dermabond can be effectively used on a wide array of wound types and sizes, from minor cuts to larger incisions.
- Hypoallergenic Formulation: Formulated to be hypoallergenic, it lowers the risk of allergic reactions in patients.
- Cost-Efficiency: Despite potentially higher upfront costs compared to traditional sutures, Dermabond may lead to long-term savings due to reduced follow-up care and removal procedures.
What is Liquid Bandage
Liquid bandage is a convenient and effective solution for minor cuts, abrasions, and blisters. Composed of cyanoacrylate and other polymers, it forms a flexible, waterproof seal over the wound, providing a protective barrier against infection.
Applied directly to the skin, it dries quickly and stays in place, making it particularly useful for areas prone to movement. Its ease of use and availability over-the-counter make it a popular choice for at-home first aid.
As the wound heals, the liquid bandage naturally wears off or can be easily removed with an acetone-based nail polish remover. Its versatility and simplicity make it a valuable addition to any basic first aid kit.
Applying a liquid bandage is a swift process, with only a mild stinging sensation upon application. It effectively seals the wound with just one application, minimizing the risk of infection due to the secure closure.
These bandages are also water-resistant, allowing you to shower or bathe without concern. The seal remains intact for a period of 5 to 10 days, after which it naturally detaches once its purpose is served.
In certain instances, it may be advisable to consult your healthcare provider before reapplying the liquid bandage after the seal has fallen off. However, for most minor cuts, significant healing will have occurred by this point.
Additionally, using these products can potentially reduce the size of resulting scars at the injury site. Liquid skin adhesives are readily available at your local pharmacy. There are many brands of liquid bandages ranging in prices.

can be found at walmart for around $2.97

found a cvs for $7.49

found at walgreens for $8.49
Applying and Caring for a Liquid Bandage.
1. Begin by ensuring your hands or a clean towel are thoroughly washed. Clean the cut and the surrounding area with cold water and soap, then pat it dry with a clean towel or gauze pad. It’s crucial that the site is completely dry.
2. Remember, the liquid bandage should be applied on top of the skin, not inside the wound. Gently bring the cut together with your fingers to create a seal.
3. Apply the liquid bandage over the cut, spreading it from one end to the other to cover it entirely. Hold the cut together for approximately a minute to allow the adhesive to dry.
4. Avoid using liquid bandage near the eyes, ears, nose, or internally in the mouth. If applied accidentally in any of these areas, seek medical attention promptly.
5. Once the liquid adhesive has dried, it’s safe to bathe. However, refrain from scrubbing the site, as this could loosen the seal or remove the adhesive altogether. You can wash the site daily with soap and water to maintain cleanliness and prevent infection. Pat the site dry after washing.
6. Do not use any other ointments on the cut site, as this can weaken the bond and slow down the healing process.
7. Resist the urge to scratch or scrub the site, as this can remove the liquid bandage.
Remember these important points:
- Minimize activity to prevent the wound from reopening.
- Keep your hands clean while caring for the wound.
- Proper wound care can help reduce scarring.
- If you have any questions or concerns about caring for stitches or staples at home, contact your healthcare provider.
- Pain medicine like acetaminophen can be taken as directed for pain at the wound site.
- Follow up with your provider to ensure the wound is healing properly.
When to call a doctor
Call your doctor or provider right away if:
- There is any redness, pain, or yellow pus around the injury. This could mean there is an infection.
- There is bleeding at the injury site that will not stop after 10 minutes of direct pressure.
- You have new numbness or tingling around the wound area or beyond it.
- You have a fever of 100°F (38.3°C) or higher.
- There is pain at the site that will not go away even after taking pain medicine.
- The wound has split open.
Comparison between liquid Bandage and Dermabond
| Dermabond (2-octyl cyanoacrylate) | Liquid Bandages |
|---|---|
| Surgical incision closure, lacerations | Minor cuts, abrasions, blisters |
| 2-octyl cyanoacrylate | Various formulations (often cyanoacrylate-based) |
| High tensile strength, designed for medical use | Moderate tensile strength, suitable for minor wounds |
| Applied by healthcare professionals | Applied by consumers directly |
| Polymerizes quickly upon contact with moisture, forming a strong bond | Polymerizes quickly, forming a protective film |
| Forms a thicker, stronger film | Forms a thinner, more flexible film |
| Strong barrier against infection, designed to hold wound edges together | Provides a barrier against infection, primarily protects minor wounds |
| Typically lasts 5-10 days before sloughing off naturally | Lasts a few days, may require reapplication depending on the wound |
| Flexible but strong, can move with skin without breaking | Very flexible, but may be less durable than Dermabond |
| Naturally sloughs off as the skin heals | Naturally sloughs off, but may require reapplication if damaged |
| Requires application by a healthcare provider | Typically applied by individuals at home |
| Closing surgical incisions, deeper cuts, and lacerations | Covering minor cuts, abrasions, blisters, and small wounds |
Liquid Bandage:
- Composition: Liquid bandage is typically made from a mixture of cyanoacrylate, which is a type of adhesive, along with other ingredients like polymers and solvents. It forms a flexible, waterproof seal when applied to the skin.
- Application: Liquid bandage is applied directly to the wound. It typically comes in a small bottle with an applicator brush or a spray form. It is usually available over-the-counter and can be used at home.
- Use: It’s commonly used for minor cuts, abrasions, and blisters. It’s not suitable for deep or gaping wounds. It’s also used for surgical incisions that have been closed with sutures.
- Flexibility: Liquid bandage is more flexible and moves with the skin, which can make it more comfortable in areas that experience a lot of movement.
- Removal: It gradually wears off over time and can be easily peeled off or dissolved with an acetone-based nail polish remover.
Dermabond:
- Composition: Dermabond is a brand name for a type of skin adhesive that contains 2-octyl cyanoacrylate, which is a variant of cyanoacrylate specifically designed for medical use.
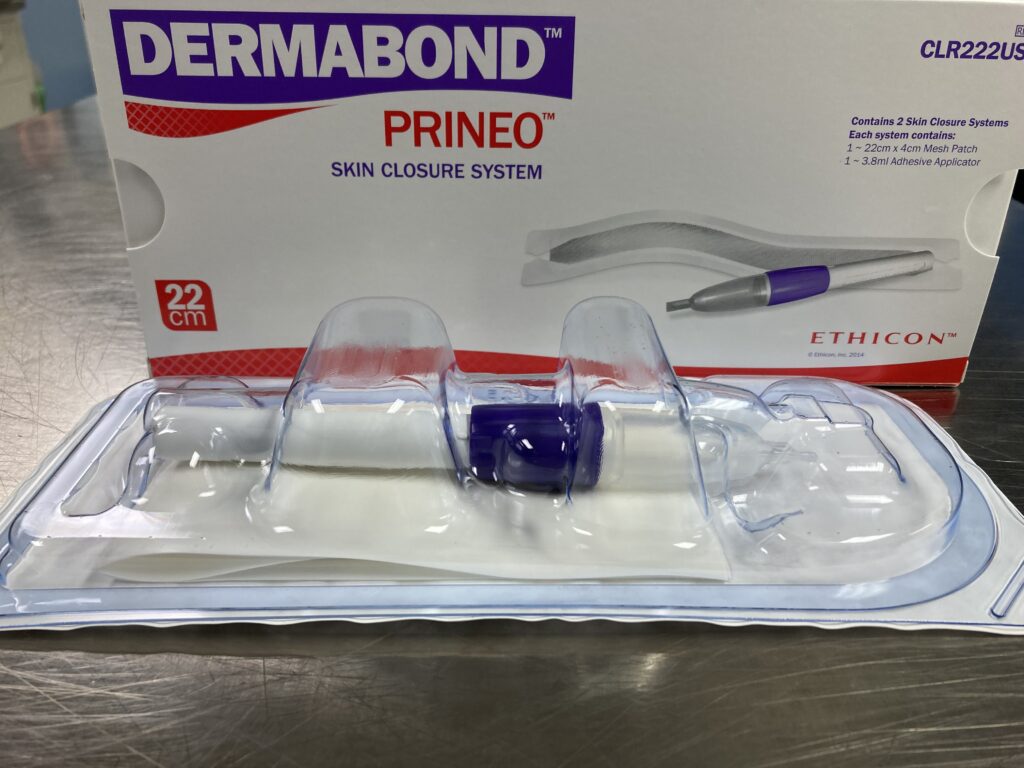
- Application: It is applied directly to the wound, much like liquid bandage. It is usually available in sterile single-use ampules.
- Use: Dermabond is often used in medical settings, such as hospitals and clinics, and is typically applied by healthcare professionals. It’s suitable for a wider range of wounds, including surgical incisions, lacerations, and puncture wounds.
- Strength: It tends to provide a stronger, more secure bond compared to some over-the-counter liquid bandages.
- Flexibility: It is less flexible than some liquid bandages, which can be a consideration for wounds in areas that experience a lot of movement.
- Removal: It naturally sloughs off as the wound heals, and it does not need to be manually removed.
DERMABOND PEN

In summary, both liquid bandage and Dermabond serve similar purposes, but Dermabond is typically used in clinical settings for more serious wounds due to its higher strength and reliability. Liquid bandage is more commonly used for minor wounds and is available for home use. Always follow the instructions provided by healthcare professionals or on the product packaging when using these products.

Above is a dermabond price range from $22 and up

Liquid bandage $10.49 at your drug store.you can find cheaper brands if you shop around.
How They Work: Mechanism of action for Dermabond vs Liquid Bandage
Dermabond (2-octyl cyanoacrylate):
- Polymerization Reaction:
- Dermabond is a type of cyanoacrylate adhesive, specifically 2-octyl cyanoacrylate. When applied to the skin, it undergoes a polymerization reaction triggered by exposure to moisture (such as water, blood, or even the natural moisture in the skin). This reaction causes the monomer molecules in the adhesive to link together, forming a strong, flexible polymer.
- Wound Closure:
- The polymerized adhesive forms a film over the wound, holding the edges together. This creates a barrier that protects the wound from contamination and helps promote healing by keeping the wound edges approximated.
- Protection and Healing:
- Dermabond forms a protective layer that shields the wound from bacteria and other contaminants. It is also designed to naturally slough off the skin as the wound heals, typically within 5 to 10 days.
Liquid Bandages (often containing cyanoacrylate):
- Application and Drying:
- Liquid bandages are typically applied by brushing or spraying the solution over the wound. Once applied, they dry quickly, forming a thin, transparent film over the wound site.
- Barrier Formation:
- Like Dermabond, the adhesive in liquid bandages creates a protective barrier over the wound. This barrier helps prevent infection, keeps dirt and debris out, and reduces the risk of irritation.
- Wound Sealing:
- Liquid bandages can help seal minor cuts, abrasions, and blisters, allowing the skin underneath to heal without the need for traditional bandages or dressings.
- Moisture Retention:
- The film created by liquid bandages helps retain moisture in the wound area, which can promote faster healing.
In summary:
- Both Dermabond and liquid bandages work by forming a protective polymer layer over wounds through a polymerization reaction. This layer helps to close the wound, protect it from infection, and promote healing while being flexible enough to move with the skin. The key difference is that Dermabond is specifically designed for medical use in closing surgical incisions and deeper wounds, while liquid bandages are generally used for more minor cuts and abrasions.
Potiential side effects and risks of Dermabond vs liquid bandages
Dermabond (2-octyl cyanoacrylate):
- Allergic Reactions:
- Dermabond can cause allergic reactions in some individuals, although this is rare. Symptoms may include redness, itching, or swelling around the application site.
- Skin Sensitivity:
- Individuals with sensitive skin may experience irritation or a mild rash. In very rare cases, a more severe reaction can occur.
- Infection Risk:
- The risk of infection is low, but it can increase if Dermabond is applied improperly or if it is used on an already infected wound.
- Delayed Healing:
- Although uncommon, improper application of Dermabond, especially on deep wounds, may result in delayed wound healing.
- Wound Dehiscence:
- If the adhesive bond isn’t strong enough or if applied incorrectly, there is a risk that the wound may reopen, a condition known as wound dehiscence.
- Thermal Sensation:
- Some patients report a warming or mild burning sensation during the polymerization process, which is typically mild and temporary.
- Tissue Damage:
- Accidental application to areas other than the wound, such as inside the wound or on mucous membranes, can cause tissue damage.
- Scarring:
- While Dermabond generally reduces scarring by keeping wound edges tightly closed, improper use or application to areas that are highly mobile can lead to more noticeable scarring.
- Application Site Issues:
- If Dermabond is applied to areas with hair, it may cause discomfort or pain when the adhesive naturally sloughs off.
- Chemical Burns:
- Although very rare, there is a risk of chemical burns if Dermabond comes into contact with the eyes or mucous membranes.
- Contraindications:
- Dermabond should not be used on infected wounds, deep puncture wounds, animal bites, or mucosal surfaces (like the mouth or inside the nose).
- Removal Issues:
- Dermabond typically sloughs off naturally as the wound heals. However, if improperly applied, medical removal may be necessary, which could be uncomfortable.
Liquid Bandages:
- Allergic Reactions:
- Liquid bandages can cause mild allergic reactions, such as itching, redness, or irritation at the application site, particularly in individuals with sensitive skin or allergies to adhesives.
- Skin Sensitivity:
- Some people may experience irritation or a mild rash, especially if they have sensitive skin or if the liquid bandage is used frequently in the same area.
- Infection Risk:
- The risk of infection is generally low, but it can increase if the liquid bandage is applied to an unclean wound or if it’s used on an already infected wound.
- Delayed Healing:
- There is a possibility of delayed healing if a liquid bandage is applied to a wound that hasn’t been thoroughly cleaned or if it is a deeper wound that requires more than just surface closure.
- Wound Dehiscence:
- Although less likely with liquid bandages than with Dermabond, there is still a risk of the wound reopening if the product does not adhere properly or if the wound is under tension.
- Thermal Sensation:
- Some formulations of liquid bandages may cause a brief stinging or warming sensation when applied, usually mild and temporary.
- Tissue Damage:
- Tissue damage is uncommon but can occur if the liquid bandage is accidentally applied to sensitive areas like the eyes or mucous membranes.
- Scarring:
- Liquid bandages typically do not affect scarring, but repeated use on the same area could lead to mild scarring or irritation.
- Application Site Issues:
- If applied to areas with hair, liquid bandages may cause discomfort when the film naturally sloughs off or if it pulls on hair.
- Chemical Burns:
- There is a possibility of mild chemical burns if liquid bandages are applied to sensitive areas, such as the eyes or mucous membranes.
- Contraindications:
- Liquid bandages should not be used on infected wounds, deep puncture wounds, or in areas where the skin is prone to frequent movement or moisture, as this can reduce effectiveness.
- Removal Issues:
- Liquid bandages typically slough off naturally but may need to be removed if they cause irritation or if they do not adhere properly. Reapplication may be necessary if the film is damaged.
Both Dermabond and liquid bandages are generally safe for their intended uses, but they carry specific risks and potential side effects that should be considered, especially in individuals with sensitive skin or specific wound types. Proper application and following instructions are crucial to minimizing these risks.
When Should you not Use Liquid Bandage?
Liquid bandages are convenient and effective for sealing minor cuts and abrasions, but there are certain situations where they should not be used:
- Deep or Large Wounds: Liquid bandages are not suitable for deep cuts, large wounds, or wounds with heavy bleeding. These types of injuries require medical attention and possibly sutures or other professional treatment.
- Infected Wounds: If the wound shows signs of infection (redness, swelling, pus, or warmth), do not use a liquid bandage. Covering an infected wound can trap bacteria inside, potentially worsening the infection.
- Animal Bites: Wounds from animal bites can be prone to infection and may require antibiotics. Liquid bandages should not be used on these types of wounds.
- Burns: Liquid bandages are not recommended for use on burns, especially severe or large burns. Burns need to be treated with appropriate burn care methods, and covering them with a liquid bandage can hinder healing or cause further irritation.
- Allergic Reactions: If you have a known allergy to any of the ingredients in the liquid bandage, avoid using it. Signs of an allergic reaction might include itching, redness, or rash at the application site.
- Mucous Membranes and Sensitive Areas: Do not apply liquid bandages on mucous membranes (like inside the mouth or nose) or near the eyes. These areas are sensitive, and liquid bandages can cause irritation or discomfort.
- Joint Areas: Liquid bandages are not ideal for wounds over joints (like knuckles or elbows) because the movement can cause the bandage to crack or peel off prematurely.
In such cases, traditional bandages, medical attention, or other appropriate wound care methods should be considered.
Frequently Asked Questions and answers about Dermabond
1. What is Dermabond?
Dermabond is a sterile, liquid adhesive used to close small wounds and surgical incisions. It acts as a skin glue, forming a strong bond across wound edges to help the skin heal naturally.
2. How does Dermabond work?
Dermabond polymerizes when applied to the skin, creating a protective layer that holds the wound edges together. It dries quickly and typically remains on the skin for 5-10 days until it naturally falls off as the wound heals.
3. Is Dermabond safe for all types of wounds?
Dermabond is suitable for small, clean, and straight wounds. It is not recommended for deep, jagged, or heavily contaminated wounds, nor for areas of high movement, tension, or moisture, such as joints.
4. How should I care for a wound sealed with Dermabond?
Keep the area dry for at least 24 hours. After that, gentle washing is acceptable, but avoid scrubbing the area. Do not apply ointments, lotions, or bandages directly over the Dermabond unless instructed by a healthcare provider.
5. Can I shower after receiving Dermabond?
Yes, but you should avoid soaking the wound in water. Quick showers are generally fine after the first 24 hours, but avoid hot tubs, swimming pools, or baths.
6. What if the Dermabond starts peeling off early?
If Dermabond starts peeling off before the wound is fully healed, consult your healthcare provider. Do not pull at it, as this could reopen the wound.
7. Is Dermabond painful to apply?
Most patients feel a brief sting when Dermabond is first applied, similar to applying rubbing alcohol. The sensation usually fades quickly.
8. What should I do if I have an allergic reaction to Dermabond?
Allergic reactions to Dermabond are rare but possible. Symptoms include redness, itching, swelling, or rash around the application site. If you experience these, contact your healthcare provider immediately.
Frequently Asked Questions and answers about Liquid Bandages
1. What is a liquid bandage?
A liquid bandage is a topical skin treatment that forms a protective, flexible layer over minor cuts, scrapes, and blisters, promoting healing and protecting the area from dirt and germs.
2. How do I apply a liquid bandage?
Clean the wound area thoroughly before application. Apply a thin layer of the liquid bandage over the wound and allow it to dry completely. Reapply as needed according to the product instructions.
3. Can liquid bandages be used on all types of wounds?
Liquid bandages are suitable for small, superficial cuts, scrapes, and blisters. They are not recommended for deep wounds, punctures, infected areas, or burns. For serious injuries, consult a healthcare provider.
4. How long does a liquid bandage last?
A liquid bandage typically lasts for several days, depending on the product and the location of the wound. It will naturally wear off as the skin heals or can be reapplied if needed.
5. Can I use a liquid bandage on my face or near my eyes?
Yes, liquid bandages can be used on the face but should be kept away from the eyes, mouth, and nose. If contact occurs, rinse thoroughly with water and seek medical attention if irritation persists.
6. What should I do if I experience irritation or an allergic reaction?
If you experience redness, itching, or a rash after applying a liquid bandage, discontinue use and wash the area with soap and water. If symptoms persist, contact a healthcare provider.
7. Can I apply a liquid bandage over an ointment or cream?
No, liquid bandages should be applied directly to clean, dry skin. Ointments and creams can prevent the bandage from adhering properly and reduce its effectiveness.
8. Can liquid bandages be used on children?
Yes, many liquid bandages are safe for use on children. However, always read the product label for age recommendations and consult with a healthcare provider if you have concerns.
Clarifications and Common Concerns
1. Are Dermabond and liquid bandages the same?
No, Dermabond is a medical-grade adhesive used primarily for surgical incisions and certain types of wounds under medical supervision, whereas liquid bandages are over-the-counter products for minor skin injuries.
2. Can these products be used interchangeably?
No, they have different applications and strengths. Dermabond is used for more significant wounds and typically under the guidance of a healthcare provider, while liquid bandages are for minor cuts and scrapes.
3. Will using these products leave scars?
Both products are designed to minimize scarring, but the likelihood of scarring depends on the wound’s size, depth, and location, as well as individual healing factors.
4. What should I do if the wound reopens after using these products?
If a wound reopens after applying Dermabond or a liquid bandage, seek medical advice, especially if the wound is deep or bleeds heavily.
If you have further questions or concerns, it’s always best to consult a healthcare provider for personalized advice.
Resources:
Work experiences as an RN