Arterial disease and venous disease are two distinct types of circulatory disorders that affect blood vessels in the body. They involve different parts of the vascular system and have distinct causes, symptoms, and treatments.
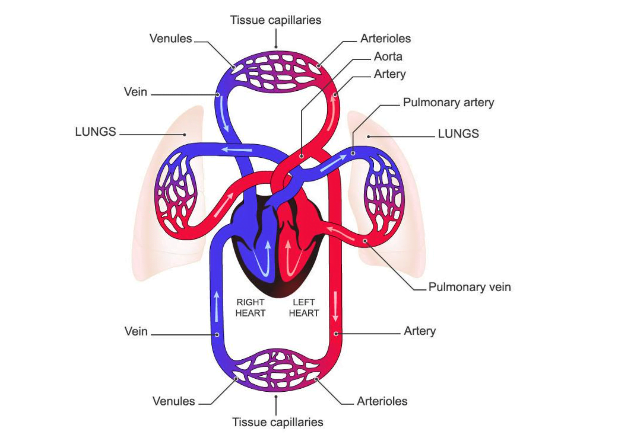
Arterial disease, also known as artery disease, is a condition that impacts the arteries in your body. These arteries are responsible for carrying oxygen-rich blood from your heart to the tissues throughout your body. Venous disease refers to any condition that impacts your veins, crucial vessels responsible for circulating blood throughout your body by transporting it back to the heart.
Key differences between arterial disease and venous disease.
| Arterial Disease | Venous Disease |
|---|---|
| Affects arteries, carrying oxygen-rich blood away from the heart | Affects veins, responsible for returning deoxygenated blood to the heart |
| Involves issues with blood flow away from the heart | Involves problems with blood flow toward the heart |
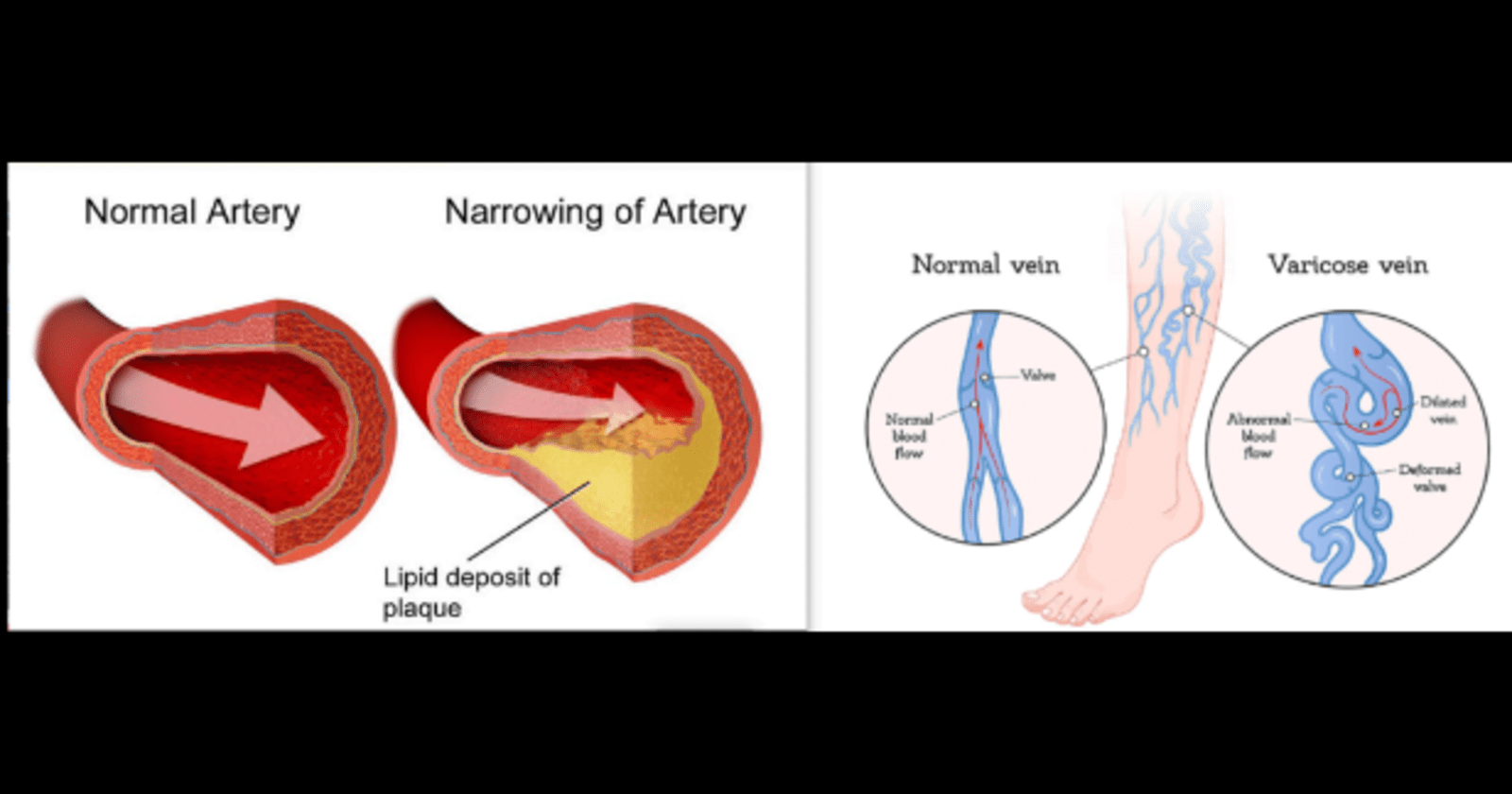
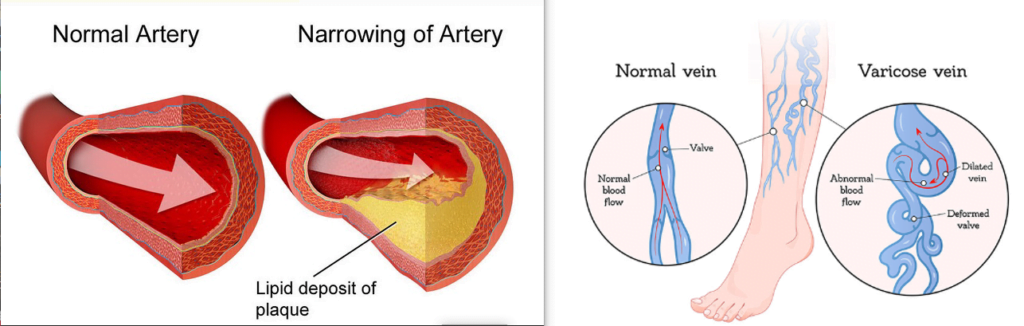
| Can lead to conditions like atherosclerosis, peripheral artery disease, potentially causing reduced blood flow, ischemia, or infarction | May manifest as conditions like varicose veins, deep vein thrombosis (DVT), or chronic venous insufficiency, causing issues related to blood pooling and impaired return to the heart |
| Often associated with high blood pressure, high cholesterol, smoking, and diabetes | Risk factors may include prolonged immobility, obesity, family history, and conditions affecting blood clotting |
| Involves lifestyle modifications, medications to control risk factors, and surgical interventions like angioplasty or bypass surgery | Treatment may include compression therapy, medications, lifestyle changes, and procedures like vein ablation or thrombectomy |
Causes Of Arterial Disease.
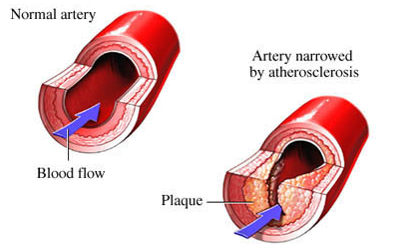
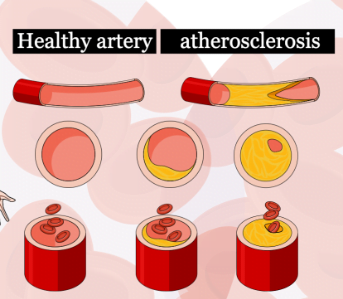
Arterial diseases often result from atherosclerosis, a condition characterized by the build-up of plaque (fat, cholesterol, and other substances) on the inner walls of arteries. This can lead to narrowing or blockage of the arteries, reducing blood flow.
Steps/stages of arterial disease.
- Endothelial Dysfunction:
- The process often begins with damage to the inner lining (endothelium) of the arteries.
- Factors such as high blood pressure, smoking, diabetes, and inflammation can cause endothelial dysfunction.
- Dysfunctional endothelial cells are less capable of regulating vasodilation, maintaining a smooth surface, and preventing clot formation.
- Formation of Fatty Streaks:
- Lipids, especially low-density lipoprotein (LDL) cholesterol, infiltrate the damaged endothelium.
- These lipids accumulate in the arterial wall, particularly in areas prone to turbulence or injury (e.g., branch points).
3. Inflammatory Response:
- The presence of lipids triggers an inflammatory response.
- White blood cells (macrophages) migrate to the site, engulfing lipids and forming foam cells.
- Inflammation contributes to further damage and attracts more immune cells.
4. Formation of Plaque:
- Foam cells and smooth muscle cells in the arterial wall contribute to the formation of atherosclerotic plaque.
- Plaque is composed of lipids, cellular debris, calcium deposits, and fibrous tissue.
5. Narrowing of Arteries:
- As the plaque grows, it protrudes into the arterial lumen, narrowing the vessel.
- This narrowing, known as stenosis, reduces blood flow and oxygen delivery to tissues.
6. Plaque Rupture and Thrombosis:
- Plaques can become unstable and prone to rupture.
- If a plaque ruptures, it exposes the underlying tissue to the bloodstream, triggering the formation of blood clots (thrombosis).
- Clots can partially or completely obstruct blood flow.
7. Ischemia and Tissue Damage:
- Reduced blood flow and oxygen supply lead to ischemia in tissues supplied by the affected arteries.
- Ischemia can result in damage to organs and tissues, compromising their function.
8. Complications:
- Arterial diseases can lead to various complications, such as myocardial infarction (heart attack) in the case of coronary arteries or limb ischemia in peripheral arteries.
9. Adaptive Remodeling:
- Arteries may undergo adaptive remodeling in response to plaque formation, attempting to maintain blood flow.
- However, this remodeling may not be sufficient to prevent the negative consequences of advanced atherosclerosis.
Types of Arterial Diseases
There are several types of arterial diseases, each with its own characteristics and impact on health. Some common types include:
- Atherosclerosis:
- Atherosclerosis is a condition characterized by the buildup of plaques (composed of cholesterol, fat, and other substances) on the inner walls of arteries. This can lead to narrowing and hardening of the arteries, reducing blood flow to vital organs and tissues.
- Peripheral Artery Disease (PAD):
- PAD occurs when there is atherosclerosis in the arteries that supply blood to the limbs, usually the legs. This can result in symptoms such as leg pain, numbness, and difficulty walking.
- Coronary Artery Disease (CAD):
- CAD is a type of atherosclerosis that affects the arteries supplying blood to the heart muscle. It can lead to angina (chest pain), heart attacks, and other cardiovascular complications.
- Carotid Artery Disease:
- This condition involves the buildup of plaques in the carotid arteries, which supply blood to the brain. Carotid artery disease increases the risk of stroke, as plaques may break loose and travel to the brain, causing a blockage.
- Renal Artery Stenosis:
- Narrowing of the renal (kidney) arteries due to atherosclerosis can result in reduced blood flow to the kidneys. This can lead to hypertension (high blood pressure) and kidney problems.
- Mesenteric Artery Disease:
- Atherosclerosis affecting the arteries supplying blood to the intestines can lead to mesenteric artery disease. Symptoms may include abdominal pain after eating and weight loss.
- Raynaud’s Disease:
- Raynaud’s disease involves the narrowing of smaller arteries that supply blood to your skin, usually in the fingers and toes. This can lead to color changes in the affected areas and may cause pain.
- Arteritis:
- Arteritis refers to inflammation of the arteries. Temporal arteritis, for example, affects the temporal arteries and can lead to headaches, jaw pain, and vision problems.
- Fibromuscular Dysplasia (FMD):
- FMD is a rare condition where the walls of medium-sized arteries develop abnormal cell growth. It can affect various arteries, including those leading to the kidneys, causing hypertension.
- Buerger’s Disease (Thromboangiitis Obliterans):
- Buerger’s disease is characterized by inflammation and clotting in small and medium-sized arteries, particularly in the hands and feet. It is strongly associated with tobacco use.
Atherosclerosis:
Atherosclerosis is a condition characterized by the buildup of plaque in the arteries, leading to a narrowing and hardening of the blood vessels. This condition is a major contributor to cardiovascular diseases, including heart attacks and strokes. The development of atherosclerosis is a complex process influenced by various factors. Elevated levels of low-density lipoprotein (LDL) cholesterol, often referred to as “bad” cholesterol, contribute to the formation of plaque in the arteries. LDL cholesterol can infiltrate the arterial walls and initiate the atherosclerotic process.
Atherosclerosis is closely linked to coronary artery disease (CAD), and the relationship between the two is fundamental to the understanding of cardiovascular health. Coronary artery disease specifically refers to the atherosclerosis that occurs in the coronary arteries, the blood vessels that supply oxygen and nutrients to the heart muscle
Peripheral Arterial Disease (PAD):
Peripheral Arterial Disease (PAD), also known as peripheral vascular disease (PVD) or peripheral artery occlusive disease, is a condition that occurs when there is a build-up of plaque in the arteries that supply blood to the extremities, usually the legs. This build-up of plaque, a fatty substance consisting of cholesterol, calcium, and other substances, can lead to a narrowing or blockage of the arteries, reducing blood flow to the limbs.
Complications:
- Critical Limb Ischemia: Severe PAD can lead to critical limb ischemia, a condition where blood flow to the limbs is severely restricted, resulting in pain at rest, ulcers, and the risk of limb loss.
- Cardiovascular Events: People with PAD are at an increased risk of heart attack and stroke.
Arterial Thrombosis:
Arterial thrombosis is a condition characterized by the formation of a blood clot (thrombus) within an artery. This can lead to the obstruction of blood flow, potentially causing serious consequences such as tissue damage, organ dysfunction, or even a life-threatening event like a heart attack or stroke. Arterial thrombosis is associated with atherosclerosis, a condition characterized by the accumulation of plaque on the inner walls of arteries.
Complications that can arise from Arterial Thrombosis
- Organ Damage: Arterial thrombosis can lead to damage of the affected organ or tissue due to reduced blood supply.
- Stroke or Heart Attack: Depending on the location of the thrombosis, a stroke or heart attack may occur.
- Peripheral Arterial Disease (PAD): Arterial thrombosis in the peripheral arteries can contribute to PAD.
Hypertension (High Blood Pressure):
- Blood pressure is the force of blood against the walls of the arteries as the heart pumps it around the body. Hypertension occurs when this pressure is consistently too high.
- Impact on Arteries: High blood pressure can damage the arteries over time. The increased pressure can lead to the thickening and hardening of the arterial walls, a condition known as arteriosclerosis.

Arteritis:
Arteritis is a medical term that refers to the inflammation of arteries, which are blood vessels responsible for carrying oxygenated blood from the heart to the rest of the body. This inflammation can affect arteries of various sizes and can lead to a range of symptoms and potential complications.
There are different types of arteritis, each characterized by specific features, affected arteries, and associated health risks. Some common types include:
- Giant Cell Arteritis (GCA): Also known as temporal arteritis, GCA typically affects the arteries in the head, especially those around the temples. It is more common in older adults and can cause symptoms such as headaches, jaw pain, and vision problems.
- Takayasu Arteritis: This form of arteritis primarily targets large arteries, particularly the aorta and its major branches. Takayasu arteritis is more common in young adults, and symptoms may include fatigue, muscle pain, and weak pulses in the limbs.
- Polyarteritis Nodosa (PAN): PAN is a rare type of arteritis that affects medium-sized arteries. It can involve multiple organs and cause symptoms such as fever, weight loss, and abdominal pain.
- Kawasaki Disease: This type of arteritis typically occurs in children and can affect medium-sized arteries, including the coronary arteries around the heart. Symptoms may include fever, rash, and swelling, and if left untreated, it can lead to serious heart complications.
Aneurysms
An aneurysm is a localized, abnormal dilation of a blood vessel, resulting from a weakened wall. Aneurysms can occur in arteries (arterial aneurysms) or veins (venous aneurysms), but the majority of cases involve arteries.
| Type of Aneurysm | Location |
|---|---|
| Thoracic Aortic Aneurysm (TAA) | Involves the aorta in the chest. |
| Abdominal Aortic Aneurysm (AAA) | Occurs in the abdominal portion of the aorta. |
| Cerebral Aneurysms | Located in the brain. |
| Peripheral Aneurysms | Affect arteries outside the heart and brain, such as those in the legs (popliteal aneurysm) or arms. |
Aneurysms can be asymptomatic and go unnoticed, or they may present with symptoms depending on their location, size, and the degree of rupture or dissection. Some common symptoms include:
- Pain: May vary depending on the location of the aneurysm.
- Pulsatile Mass: A throbbing lump may be felt near the affected artery.
- Neurological Symptoms: If a cerebral aneurysm ruptures, it can lead to symptoms such as a severe headache, nausea, vomiting, and neurological deficits.
Aneurysms are often diagnosed through imaging studies like ultrasound, CT scans, or MRIs. Treatment options depend on factors such as the size, location, and risk of rupture. Options include:
- Monitoring: Small, stable aneurysms may be monitored regularly without intervention.
- Medication: Control of blood pressure and other risk factors.
- Surgery: Surgical procedures may involve the placement of a graft to reinforce the weakened vessel wall.
- Endovascular Repair: A less invasive approach where a stent or graft is inserted through blood vessels to the site of the aneurysm.
The risk of rupture is a serious concern, as it can lead to internal bleeding and life-threatening complications.
Raynaud’s Disease
Raynaud’s phenomenon or Raynaud’s syndrome, is a condition that affects blood flow to certain parts of the body — usually the fingers and toes. This phenomenon occurs when smaller arteries that supply blood to your skin constrict excessively in response to cold or stress, limiting blood supply to affected areas (vasospasm).
Here are some key details about Raynaud’s disease:
- Symptoms:
- Color Changes: Skin in affected areas, usually fingers and toes, might turn white or blue in response to cold or stress. As blood flow returns, the skin may turn red.
- Numbness or Tingling: In addition to color changes, affected areas might feel numb or tingly.
- Throbbing or Swelling: In some cases, affected areas may throb and swell.
- Episodic Nature: Episodes of vasospasm can last from minutes to hours, and the frequency of attacks can vary from person to person.
- Triggers:
- Cold Weather: Exposure to cold temperatures is a common trigger.
- Stress: Emotional stress or tension can trigger an episode.
- Smoking: Nicotine can cause blood vessels to constrict.
- Types of Raynaud’s:
- Primary (or idiopathic) Raynaud’s: This is the more common form and isn’t usually related to any other medical condition. It tends to be less severe.
- Secondary (or secondary to other diseases) Raynaud’s: This form, also known as Raynaud’s phenomenon, is less common but more serious. It is often associated with other diseases, such as scleroderma or lupus.
Complications:
- Severe cases of Raynaud’s can lead to ulcers or sores on the affected areas.
- In rare cases, it can cause deformities of the fingers and toes.
Coronary Artery Disease (CAD):
Coronary Artery Disease (CAD), also known as ischemic heart disease or coronary heart disease, is a medical condition that occurs when the blood vessels supplying the heart muscle (coronary arteries) become narrowed or blocked. The coronary arteries are responsible for delivering oxygen and nutrients to the heart muscle, and when they are affected by CAD, it can lead to various complications.
Here are some key points about Coronary Artery Disease:
- Atherosclerosis: CAD is primarily caused by atherosclerosis, a condition where fatty deposits, cholesterol, calcium, and other substances build up on the inner walls of the coronary arteries. Over time, this buildup can form plaques, causing the arteries to become narrow and restricting blood flow.
- Reduced Blood Flow: As the coronary arteries narrow, the blood flow to the heart muscle is diminished. This reduction in blood flow can lead to angina (chest pain or discomfort) or, in severe cases, myocardial infarction (heart attack).
- Risk Factors: Several risk factors contribute to the development of CAD. These include:
- Age: Risk increases with age.
- Gender: Men are generally at a higher risk, but women’s risk increases after menopause.
- Family history: A family history of CAD can increase the risk.
- Smoking: Tobacco smoke contains chemicals that can damage blood vessels and contribute to atherosclerosis.
- High blood pressure: Hypertension can accelerate the progression of atherosclerosis.
- High cholesterol levels: Elevated levels of LDL (“bad”) cholesterol and low levels of HDL (“good”) cholesterol can contribute to plaque formation.
- Symptoms: The symptoms of CAD can vary. Common symptoms include chest pain or discomfort (angina), shortness of breath, fatigue, and in more severe cases, heart attack symptoms such as intense chest pain, nausea, and sweating.
- Diagnosis: CAD is often diagnosed through a combination of medical history, physical examination, and diagnostic tests such as electrocardiogram (ECG or EKG), stress testing, echocardiogram, and coronary angiography.
- Treatment: Treatment strategies for CAD aim to relieve symptoms, reduce the risk of complications, and improve overall heart health. Common treatments include lifestyle changes (diet, exercise, smoking cessation), medications (such as statins, antiplatelet drugs, and beta-blockers), and, in some cases, interventional procedures like angioplasty or coronary artery bypass grafting (CABG).
- Prevention: Lifestyle modifications, such as maintaining a healthy diet, regular exercise, not smoking, and managing conditions like diabetes and hypertension, can help prevent or slow the progression of CAD.
Carotid Artery Disease:
The narrowing of the carotid arteries can lead to a reduction in blood flow to the brain, increasing the risk of stroke. If a piece of the plaque breaks off or a blood clot forms in the narrowed artery and travels to the brain, it can block a smaller blood vessel, causing a stroke.
Symptoms of carotid artery disease may not be apparent until the condition becomes severe or a stroke occurs. Some common symptoms include:
- Transient Ischemic Attacks (TIAs or “mini-strokes”): These are brief episodes of stroke-like symptoms that may precede an actual stroke. They can include sudden weakness, numbness, or paralysis on one side of the body, slurred speech, and vision changes.
- Sudden Severe Headache: This may be a symptom of a severe blockage or clot in the carotid arteries.
- Trouble Speaking or Understanding Speech: Difficulty in speaking coherently or understanding spoken or written language.
- Loss of Coordination or Balance: Problems with coordination and balance can occur if blood flow to the brain is compromised.
- Drooping on One Side of the Face: Similar to the facial drooping seen in a stroke.
Several risk factors contribute to the development of carotid artery disease, including age, smoking, high blood pressure, high cholesterol, diabetes, and a family history of atherosclerosis or cardiovascular disease.
Renal Artery Stenosis:
Renal artery stenosis (RAS) refers to the narrowing of one or both renal arteries, which supply blood to the kidneys. This narrowing is often caused by the buildup of plaque or atherosclerosis, a condition where fatty deposits, cholesterol, and other substances accumulate on the inner walls of arteries.
Buerger’s Disease (Thromboangiitis Obliterans):
Buerger’s disease, also known as thromboangiitis obliterans, is a rare and inflammatory condition that primarily affects the small and medium-sized arteries and veins in the arms and legs. The exact cause of Buerger’s disease is unknown, but it is strongly associated with tobacco use, particularly cigarette smoking. The disease most commonly affects young to middle-aged men.
Key features of Buerger’s disease include:
- Peripheral Arterial Disease (PAD): Buerger’s disease is a form of peripheral arterial disease that involves inflammation and clotting in the blood vessels, leading to reduced blood flow to the extremities. This can result in pain, numbness, and tingling in the affected limbs.
- Thrombosis and Blood Clots: Blood clots, or thrombi, can form in the affected blood vessels, leading to further obstruction of blood flow. This can contribute to the symptoms and complications associated with the disease.
- Symptoms: Patients with Buerger’s disease may experience symptoms such as intermittent claudication (pain during physical activity that resolves with rest), cold extremities, skin discoloration, and, in severe cases, the development of ulcers or sores on the fingers and toes.
- Association with Smoking: Smoking is a significant risk factor for Buerger’s disease. The majority of individuals with this condition are current or former smokers. The disease is rare in nonsmokers.
- Diagnosis: The diagnosis of Buerger’s disease is based on clinical symptoms, medical history, and various tests such as angiography (imaging of blood vessels), Doppler ultrasound, and blood tests. A healthcare professional may also inquire about the patient’s smoking history.
- Treatment: The most effective treatment for Buerger’s disease is to quit smoking. Smoking cessation is crucial in preventing the progression of the disease and reducing symptoms. Other treatments may include medications to improve blood flow, pain management, and in severe cases, surgical procedures such as sympathectomy or bypass surgery.
- Prognosis: The prognosis for individuals with Buerger’s disease depends on various factors, including the extent of the disease, the severity of symptoms, and the individual’s response to treatment. Quitting smoking is essential for improving outcomes and preventing further complications.
Types of venous Disease
Venous disease refers to conditions that affect the veins, which are blood vessels responsible for carrying deoxygenated blood back to the heart.
There are various types of venous diseases, each with its own causes, symptoms, and treatments.
Varicose Veins:

Varicose veins are enlarged, swollen, and twisted veins that usually appear dark purple or blue. They often occur in the legs and can cause discomfort or pain. Varicose veins develop when the valves in the veins that are supposed to prevent the backward flow of blood become weak or damaged. This results in blood pooling in the veins, causing them to enlarge.
Symptoms of varicose veins may include:
- Pain or aching in the legs: This can be more pronounced after long periods of standing or sitting.
- Swelling: The affected leg may swell, particularly after prolonged periods of standing.
- Itching or irritation: Some people may experience itching around the veins.
- Skin changes: The skin over the veins may become discolored, and in severe cases, ulcers may develop.
Deep Vein Thrombosis (DVT):
Deep Vein Thrombosis (DVT) is a medical condition characterized by the formation of blood clots (thrombi) in the deep veins, typically in the legs. These clots can cause serious health problems if they break loose and travel to the lungs, causing a pulmonary embolism (PE), which can be life-threatening.
Key points about Deep Vein Thrombosis (DVT) include:
- Risk Factors:
- Immobility: Long periods of immobility, such as during long flights or bed rest, can increase the risk of DVT.
- Surgery or Trauma: Certain surgeries, especially joint replacement surgeries, and trauma can increase the risk of blood clot formation.
- Medical Conditions: Conditions like cancer, heart disease, and inflammatory disorders can increase the risk.
- Genetics: A family history of blood clots may contribute to an individual’s risk.
- Symptoms:
- DVT may present with symptoms such as swelling, pain, tenderness, and redness in the affected leg.
- However, it’s possible to have DVT without obvious symptoms, making it important to be aware of risk factors.
- Complications:
- The most serious complication of DVT is a pulmonary embolism (PE), where a blood clot travels to the lungs.
- Chronic complications include post-thrombotic syndrome, where there is persistent swelling and pain in the affected leg.
- Diagnosis:
- Ultrasound is a common diagnostic tool for detecting blood clots in the veins.
- Other imaging tests, such as venography or CT scans, may be used in certain cases.
- Treatment:
- Anticoagulant medications (blood thinners) are often prescribed to prevent the clot from growing and to reduce the risk of embolism.
- In some cases, procedures like thrombectomy or insertion of a vena cava filter may be necessary.
- Prevention:
- Regular movement, especially during long periods of sitting or immobility, can help prevent DVT.
- For individuals at high risk, medications or compression stockings may be recommended.
- Awareness and Education:
- It’s crucial for individuals to be aware of the risk factors and symptoms of DVT, especially if they have predisposing conditions.
- Causes and risk factors.
- Complications and potential for pulmonary embolism.
- Anticoagulant therapy and prevention strategies.
Chronic Venous Insufficiency (CVI):
Chronic Venous Insufficiency (CVI) is a medical condition that occurs when the veins in the legs are unable to pump blood back to the heart effectively. Veins have one-way valves that help blood flow against gravity, but if these valves become damaged or weakened, blood can pool in the legs, leading to various symptoms and complications.
Some common causes and risk factors for CVI include:
- Age: The risk of CVI increases with age as the veins may lose elasticity and the valves may become less efficient.
- Gender: Women are more likely to develop CVI than men, possibly due to hormonal factors.
- Family history: A family history of venous problems may increase the risk of CVI.
- Prolonged sitting or standing: Jobs or lifestyles that involve long periods of sitting or standing can contribute to the development of CVI.
- Obesity: Excess body weight puts additional pressure on the veins, increasing the risk of venous insufficiency.
- Pregnancy: The increased blood volume and pressure on the pelvic veins during pregnancy can contribute to the development of CVI.
- History of blood clots: Previous deep vein thrombosis (DVT) or other blood clot-related issues may damage the veins and contribute to venous insufficiency.
Symptoms of CVI may include:
- Leg pain or aching: Often described as a dull, throbbing pain in the legs.
- Swelling: Edema or swelling, particularly in the ankles and lower legs.
- Skin changes: Discoloration, dryness, or inflammation of the skin on the legs.
- Varicose veins: Enlarged, twisted veins that are visible just beneath the surface of the skin.
- Leg cramps: Especially at night.
- Itching or tingling: Due to poor circulation and skin changes
Venous Thromboembolism (VTE):
Venous Thromboembolism (VTE) refers to a condition in which blood clots form in the veins, leading to the potential for serious complications. VTE is a combination of two related conditions: deep vein thrombosis (DVT) and pulmonary embolism (PE).
- Deep Vein Thrombosis (DVT):
- DVT occurs when a blood clot forms in a deep vein, usually in the legs. However, it can also occur in other parts of the body.
- Risk factors for DVT include prolonged immobility (such as long flights or bed rest), surgery, trauma, obesity, smoking, and certain medical conditions that affect blood clotting.
- Pulmonary Embolism (PE):
- PE is a potentially life-threatening condition that occurs when a blood clot breaks loose from its original location (usually a DVT) and travels to the lungs, blocking one of the pulmonary arteries.
- Symptoms of PE can include difficulty breathing, chest pain, rapid heart rate, and coughing up blood.
- Risk Factors for VTE:
- Immobility or prolonged bed rest.
- Major surgery or trauma.
- Cancer and cancer treatments.
- Hormone-based medications, such as birth control pills or hormone replacement therapy.
- Genetic factors that affect blood clotting.
- Age (risk increases with age).
- Obesity.
- Smoking.
- Certain medical conditions, such as inflammatory disorders.
- Prevention and Treatment:
- Prevention strategies include early mobilization after surgery, compression stockings, anticoagulant medications, and lifestyle modifications.
- Treatment typically involves anticoagulant medications (blood thinners) to prevent further clotting and reduce the risk of complications.
- In some cases, interventions like the insertion of a vena cava filter may be considered to prevent clots from traveling to the lungs.
- Complications:
- If left untreated, VTE can lead to serious complications, including chronic leg pain and swelling, recurrent blood clots, and, in severe cases, organ damage or death.
Superficial Thrombophlebitis:
Superficial thrombophlebitis is a condition characterized by inflammation and blood clot formation in the superficial veins, which are veins located close to the surface of the skin. While it can occur in any superficial vein, it most commonly affects the veins in the legs.
Key points about superficial thrombophlebitis:
- Causes: The most common cause of superficial thrombophlebitis is the formation of a blood clot (thrombus) in a superficial vein. This clot can cause inflammation and pain. It may occur spontaneously or be associated with conditions such as varicose veins, trauma to the vein, or underlying blood clotting disorders.
- Symptoms: The symptoms of superficial thrombophlebitis may include redness, warmth, swelling, and tenderness over the affected vein. The area may also feel hard or lumpy. Pain or discomfort may be present, especially when pressure is applied to the affected area.
- Risk Factors: Several factors may increase the risk of developing superficial thrombophlebitis, including a history of varicose veins, recent surgery or trauma, prolonged immobility, obesity, and conditions that affect blood clotting.
- Diagnosis: Diagnosis is often based on a physical examination and medical history. Imaging tests, such as ultrasound, may be used to confirm the presence of a blood clot and to assess the extent of the condition.
- Treatment: Treatment for superficial thrombophlebitis aims to relieve symptoms and prevent complications. This may involve the use of nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation, compression stockings to reduce swelling, and warm compresses. In some cases, anticoagulant medications may be prescribed to prevent the clot from extending into deeper veins.
- Complications: While superficial thrombophlebitis is generally a benign condition, complications can occur. The clot may extend into deeper veins, leading to a condition called deep vein thrombosis (DVT). There is also a risk of infection at the site of the inflamed vein.
- Prognosis: With appropriate treatment, superficial thrombophlebitis often resolves within a few weeks. However, individuals with recurrent or extensive cases may require further evaluation to identify and address underlying causes
May-Thurner Syndrome:
May-Thurner Syndrome, also known as iliac vein compression syndrome, is a vascular condition characterized by the compression of the left iliac vein by the overlying right iliac artery. This compression can lead to reduced blood flow in the left iliac vein, causing symptoms such as pain, swelling, and deep vein thrombosis (DVT) in the left leg.
The anatomy of the pelvic vessels, specifically the position of the right iliac artery over the left iliac vein, makes individuals more susceptible to this syndrome. The compression can cause chronic irritation and damage to the venous wall, increasing the risk of blood clot formation.
Common symptoms of May-Thurner Syndrome may include:
- Leg pain: Typically on the left side, which may be persistent or worsen with standing or walking.
- Swelling: Swelling of the left leg or other related symptoms of venous insufficiency.
- Deep vein thrombosis (DVT): Formation of blood clots in the left iliac vein, which can be a serious complication.
Venous Ulcers
Venous ulcers, also known as venous stasis ulcers or varicose ulcers, are open sores that develop on the skin, usually in the lower legs. These ulcers are a result of poor blood circulation in the veins, typically caused by venous insufficiency. Venous insufficiency occurs when the valves in the veins of the legs are damaged or weakened, leading to blood pooling in the veins instead of flowing back to the heart.
Key points about venous ulcers:
- Causes:
- Venous Insufficiency: The most common cause is chronic venous insufficiency, where the valves in the veins are unable to prevent blood from flowing backward.
- Deep Vein Thrombosis (DVT): Blood clots in the deep veins can lead to venous insufficiency and, subsequently, venous ulcers.
- Varicose Veins: Enlarged and twisted veins can contribute to venous insufficiency and ulcer formation.
- Symptoms:
- Open Sores: Ulcers typically occur on the inner part of the ankle and may be surrounded by discolored or hardened skin.
- Pain and Discomfort: Patients may experience pain, aching, or a feeling of heaviness in the affected leg.
- Swelling: Edema (swelling) in the lower legs is common.
- Diagnosis:
- A healthcare professional will perform a physical examination of the affected area.
- Doppler ultrasound may be used to assess blood flow in the veins.
- Other imaging tests, such as venography, may be employed to visualize the veins.
- Treatment:
- Compression Therapy: Wearing compression stockings helps improve blood circulation and reduce swelling.
- Elevation: Keeping the legs elevated when possible can assist in reducing edema.
- Wound Care: Proper cleaning and dressing of the ulcer are essential for healing.
- Medications: Sometimes, medications to improve blood flow or treat underlying conditions may be prescribed.
- Prevention:
- Regular exercise to promote healthy circulation.
- Maintaining a healthy weight.
- Avoiding prolonged periods of standing or sitting.
- Using compression stockings as recommended by a healthcare professional.
Lymphedema:
Lymphedema is a condition characterized by the swelling of certain body parts, typically the arms or legs, due to the accumulation of lymphatic fluid. The lymphatic system is a network of vessels and nodes that plays a crucial role in maintaining fluid balance and filtering harmful substances from the body. When the normal flow of lymph is disrupted or impaired, fluid can build up, leading to swelling.
There are two main types of lymphedema:
- Primary Lymphedema: This type is caused by a congenital malformation or dysfunction of the lymphatic system. It is relatively rare and often appears at birth or during puberty. Primary lymphedema can affect one or both limbs.
- Secondary Lymphedema: This type is more common and occurs as a result of damage to the lymphatic system. The damage may be due to surgery, radiation therapy, infection, trauma, or other conditions that affect the lymph nodes or vessels. Breast cancer treatment, for example, can sometimes lead to secondary lymphedema if lymph nodes are removed or damaged.
Symptoms of lymphedema may include:
- Swelling in one or more limbs, typically in the arms or legs.
- Feeling of heaviness or tightness in the affected limb.
- Limited range of motion in joints.
- Aching or discomfort in the affected limb.
- Recurring infections.
Management and treatment of lymphedema often involve a combination of approaches, including:
- Compression Therapy: Wearing compression garments or using bandages to help reduce swelling.
- Manual Lymphatic Drainage (MLD): A specialized massage technique that stimulates the flow of lymphatic fluid.
- Exercise: Gentle, controlled movement to encourage lymphatic drainage and improve muscle function.
- Skin Care: Proper hygiene and moisturizing to prevent infections and maintain skin health.
- Elevation: Keeping the affected limb elevated to reduce swelling.
- Complete Decongestive Therapy (CDT): A comprehensive approach that combines various strategies, including compression, MLD, exercise, and skin care.
Causes and Risk of Venous Disease
- Blood Clots (Deep Vein Thrombosis – DVT):
- Cause: Formation of blood clots in deep veins, often in the legs. Clots can travel to the lungs, causing a pulmonary embolism.
- Risk Factors:
- Prolonged immobility (long flights, bed rest)
- Surgery or trauma
- Cancer
- Obesity
- Genetic factors
- Valve Dysfunction:
- Cause: Malfunction of venous valves, leading to blood pooling and reflux.
- Risk Factors:
- Aging
- Family history
- Female gender (hormonal changes, pregnancy)
- Previous deep vein thrombosis
- Obesity
- Chronic Venous Insufficiency (CVI):
- Cause: Inability of the veins to adequately return blood from the legs to the heart, often due to valve dysfunction.
- Risk Factors:
- Varicose veins
- History of blood clots
- Family history
- Obesity
- Occupation involving prolonged standing or sitting
| Cause | Risk Factors |
|---|---|
| Deep Vein Thrombosis (DVT) Formation of blood clots in deep veins, often in the legs. | Deep Vein Thrombosis (DVT) – Prolonged immobility (long flights, bed rest) |
| – Surgery or trauma | |
| – Cancer | |
| – Obesity | |
| – Genetic factors | |
| Valve Dysfunction Malfunction of venous valves, leading to blood pooling and reflux. | Valve Dysfunction – Aging |
| – Family history | |
| – Female gender (hormonal changes, pregnancy) | |
| – Previous deep vein thrombosis | |
| – Obesity | |
| Chronic Venous Insufficiency (CVI) Inability of the veins to adequately return blood from the legs to the heart, often due to valve dysfunction. | Chronic Venous Insufficiency (CVI) – Varicose veins |
| – History of blood clots | |
| – Family history | |
| – Obesity | |
| – Occupation involving prolonged standing or sitting |
Symptoms of Arterial and Venous Disease
- Arterial Disease:
- Pain: Patients with arterial disease may experience pain, typically in the legs, during physical activity. This is known as intermittent claudication and is due to inadequate blood flow to the muscles.
- Numbness: Reduced blood supply can lead to numbness or a tingling sensation in the affected limbs.
- Tissue Damage: Severe arterial disease can result in tissue damage or non-healing wounds, as the tissues do not receive enough oxygen and nutrients.
- Venous Disease:
- Swelling: Impaired venous return can cause fluid to accumulate in the legs, leading to swelling.
- Varicose Veins: Enlarged and twisted veins near the surface of the skin, often visible as varicose veins, are common in venous disease.
- Skin Changes: Chronic venous insufficiency can cause changes in the skin, including discoloration, thickening, and the development of ulcers, especially around the ankles.
Diagnosis for Arterial Disease
- Physical Examination: The doctor may check for signs of arterial disease, such as weak or absent pulses, cool skin, or skin discoloration.
- Ankle-Brachial Index (ABI): This test compares blood pressure in your ankle with blood pressure in your arm to determine how well your blood is flowing.
- Doppler Ultrasound: This test uses sound waves to create images of blood flow in the arteries.
- Computed Tomography Angiography (CTA) or Magnetic Resonance Angiography (MRA): These imaging techniques provide detailed pictures of the blood vessels to identify any blockages or abnormalities.
- Blood Tests: Certain blood tests can provide information about cholesterol levels and markers of inflammation, which are associated with arterial disease.
- Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart and can help identify any signs of heart-related issues.
- Angiography: This involves injecting a contrast dye into the arteries and taking X-ray images to visualize blood flow and identify any blockages.
- Treadmill Testing: In some cases, a stress test on a treadmill may be performed to evaluate how well your heart responds to physical activity.
Once a diagnosis is made, treatment options may include lifestyle changes (such as diet and exercise), medications, and, in some cases, surgical interventions.
Diagnosis for Venous Disease
Diagnosing venous diseases involves a combination of medical history assessment, physical examination, and often imaging studies.
- Medical History:
- The doctor will inquire about your symptoms, including any pain, swelling, or changes in skin color.
- They may ask about risk factors such as family history, obesity, pregnancy, prolonged periods of immobility, or a history of blood clots.
- Physical Examination:
- The doctor will conduct a thorough physical examination, focusing on the affected areas.
- They may inspect the legs for signs of varicose veins, swelling, skin changes, or ulcers.
- Palpation of the legs may reveal areas of tenderness or warmth, which could be indicative of inflammation or blood clots.
- Doppler Ultrasound:
- This non-invasive imaging test uses sound waves to create images of blood flow in the veins.
- Doppler ultrasound can help diagnose conditions such as deep vein thrombosis (DVT) by visualizing blood clots or identifying valve dysfunction in the veins.
- Venous Duplex Ultrasound:
- This is a specialized form of ultrasound that combines traditional ultrasound with Doppler ultrasound.
- Venous duplex ultrasound provides detailed images of the veins and assesses blood flow, helping to identify abnormalities in the veins.
- CT or MRI Venography:
- In some cases, a CT or MRI scan may be used to visualize the veins in more detail. This can be particularly useful for evaluating the deep veins or if other imaging methods are inconclusive.
- Venous Pressure Measurements:
- In certain situations, a test called venous pressure measurements may be performed. This involves measuring the pressure in the veins to assess how well the blood is flowing back to the heart.
- Blood Tests:
- Blood tests, such as D-dimer, may be used to assess for the presence of clotting disorders or to rule out the likelihood of deep vein thrombosis.
- Phlebography:
- Invasive contrast venography may be performed in certain cases, where a contrast dye is injected into a large vein, and X-rays are taken to visualize the veins.
Treatment for arterial and venous disease
Arterial Diseases:
- Lifestyle Changes:
- Smoking Cessation: Quitting smoking is crucial as smoking damages the blood vessels and worsens arterial diseases.
- Healthy Diet: Adopting a diet low in saturated fats, cholesterol, and sodium can help manage arterial diseases.
- Medications:
- Antiplatelet Agents: Drugs like aspirin or clopidogrel may be prescribed to reduce the risk of blood clots.
- Cholesterol-lowering Medications: Statins may be used to manage high cholesterol levels.
- Blood Pressure Control:
- Medications may be prescribed to control hypertension and maintain optimal blood pressure.
- Endovascular Procedures:
- Angioplasty and Stenting: In cases of arterial blockages, a catheter with a balloon is used to widen the narrowed artery, and a stent may be placed to keep it open.
- Surgery:
- Bypass Surgery: In severe cases, bypass surgery may be performed to redirect blood flow around a blocked artery.
Venous Diseases:
- Compression Therapy:
- Compression stockings or bandages are often recommended to improve blood flow in the veins and reduce swelling.
- Elevation of Legs:
- Keeping the legs elevated when resting can help reduce swelling and improve venous circulation.
- Medications:
- Anticoagulants: Blood thinners may be prescribed to prevent blood clots in cases of deep vein thrombosis (DVT).
- Endovenous Ablation:
- Techniques like laser or radiofrequency ablation may be used to close off malfunctioning veins.
- Sclerotherapy:
- This involves injecting a solution into small varicose veins, causing them to collapse and fade.
- Vein Stripping and Ligation:
- In some cases, surgical procedures may be recommended to remove or tie off damaged veins.
- Venous Stenting:
- For cases of venous obstruction, stenting may be considered to keep the vein open.
Resources
Most of my information are obtain from experiences during my years as a registered nurse working at several different teaching and research Hospitals and Surgical facilities in the united states and abroad.
https://www.ucsfhealth.org/conditions/peripheral-artery-disease